This document provides an overview of health assessment. It discusses that health assessment aims to identify a person's specific health needs through techniques like history taking and physical examination. It evaluates an individual's health status along the health continuum.
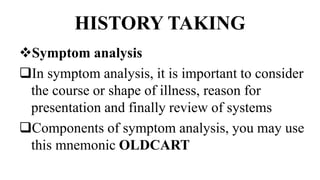
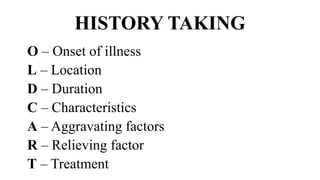
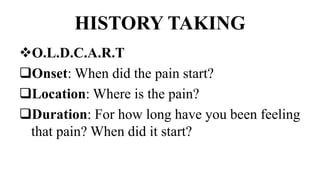
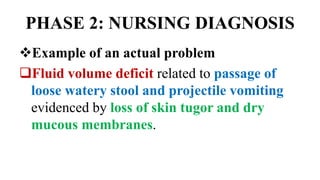
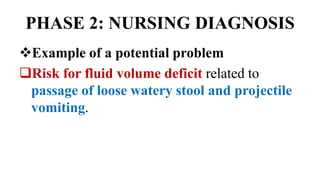
The document outlines the main components of history taking, including demographic data, presenting complaints, history of present and past illnesses, family history, social history, and occupational history. It also describes the nursing process and its phases - assessment, nursing diagnosis, planning, implementation, and evaluation. Finally, it discusses the different types of health assessments like comprehensive, focused, episodic, and screening assessments.