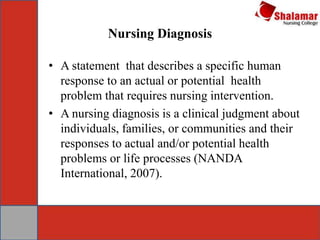
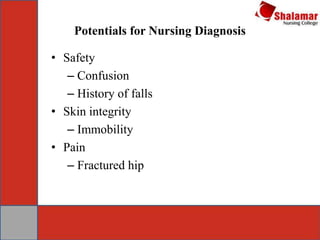
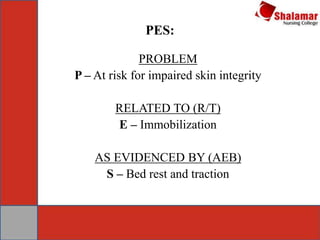
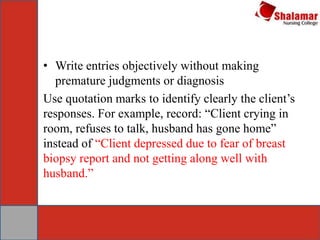
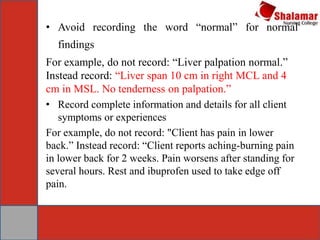
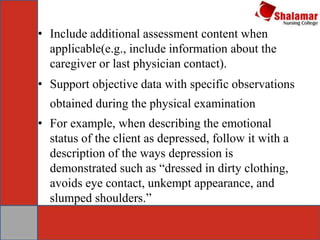
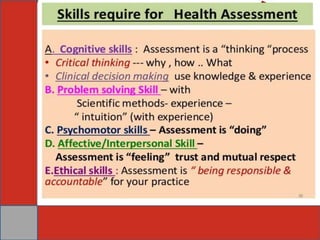
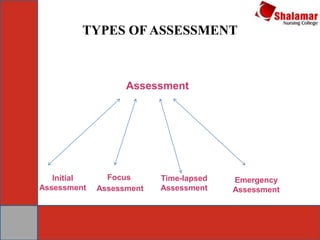
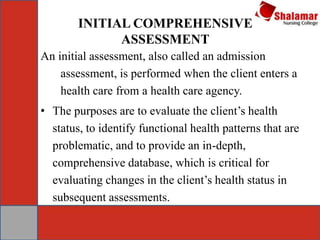
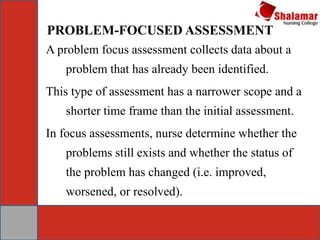
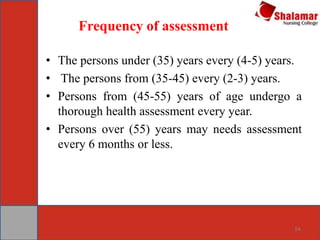
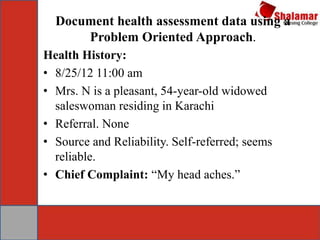
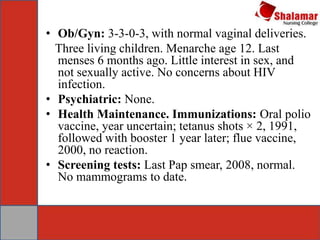
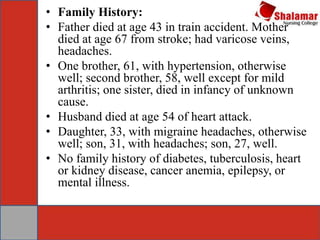
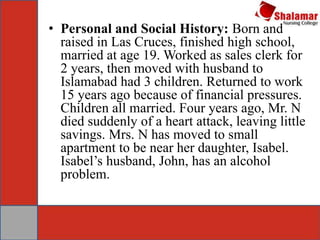
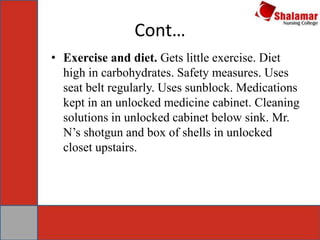
This document provides an overview of concepts related to health assessment. It defines key terms like health, assessment, data collection and diagnosis. It discusses the need for health assessment in general nursing practice and identifies different types of health assessments like initial, problem-focused, emergency and time-lapsed assessments. The document also provides examples of documenting a health assessment using a problem-oriented approach.