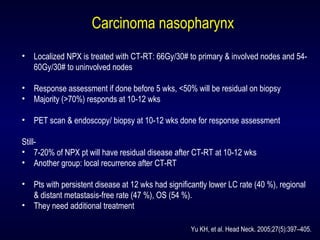
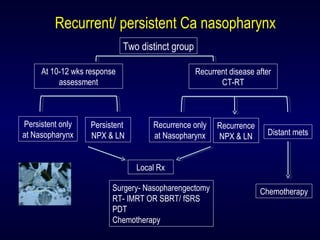
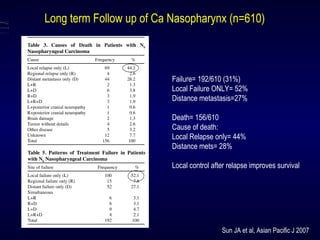
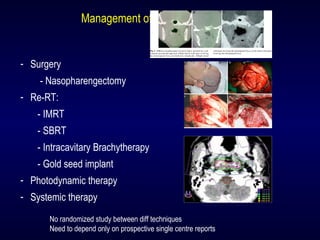
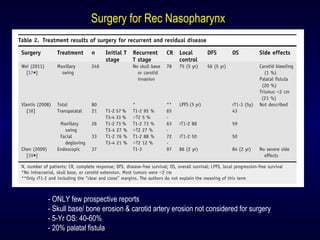
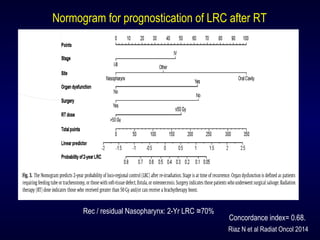
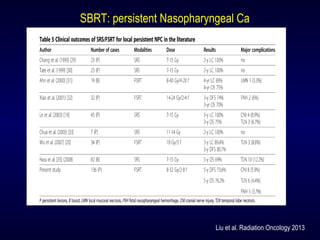
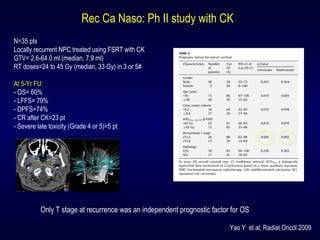
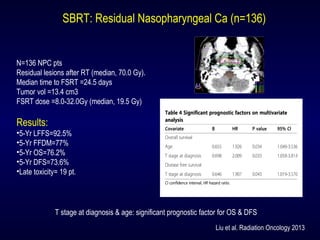
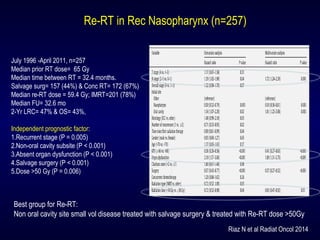
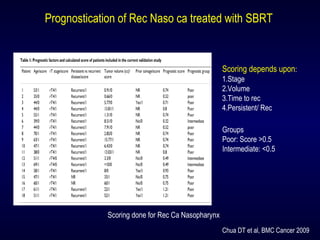
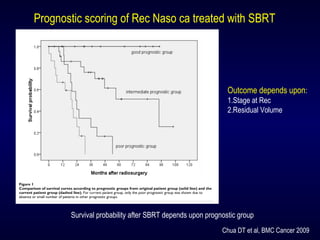
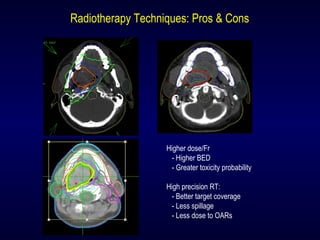
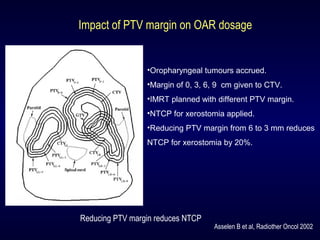
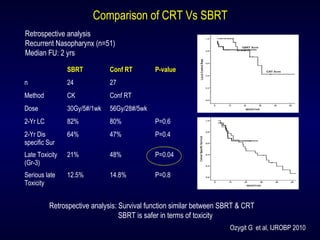
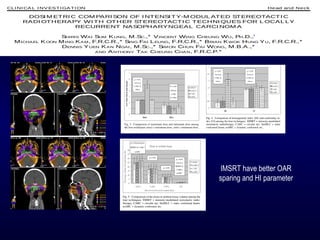
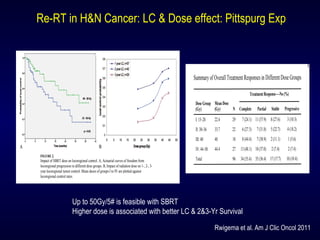
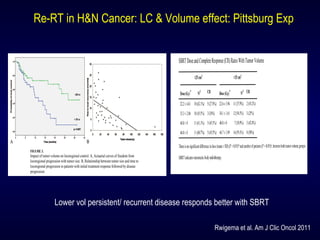
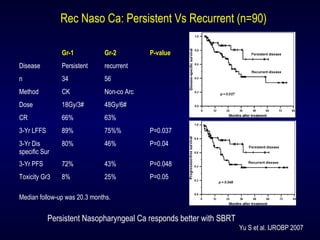
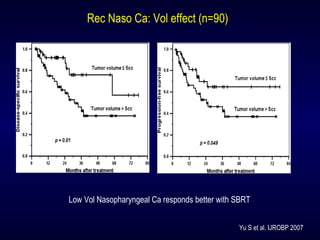
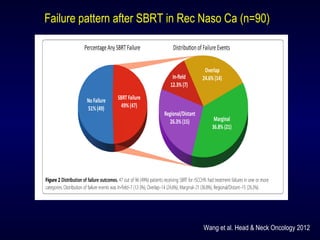
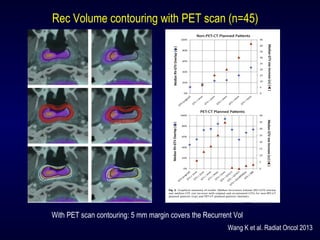
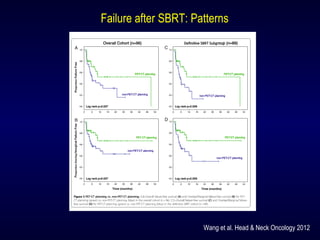
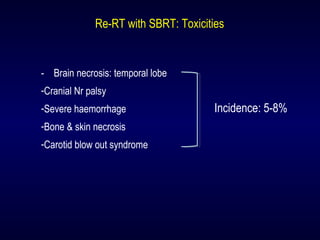
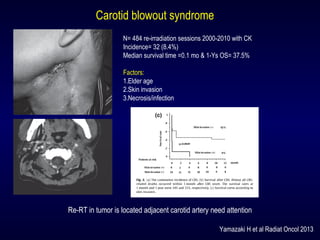
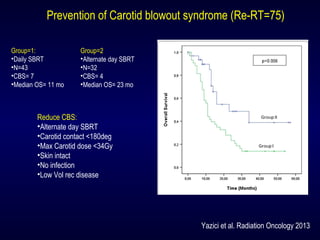
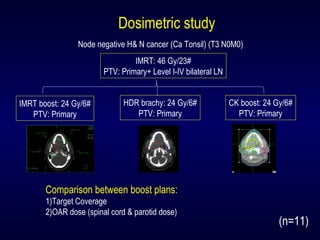
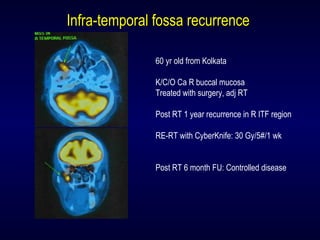
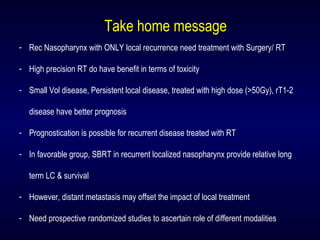
The document discusses the management of recurrent nasopharyngeal cancer, highlighting the importance of treatment options like surgery and high-precision radiotherapy. It emphasizes the significance of factors such as tumor volume, radiation dosage, and initial response time in prognostic outcomes. Additionally, it provides insights into treatment outcomes, including local recurrence rates and survival statistics for various treatment modalities.