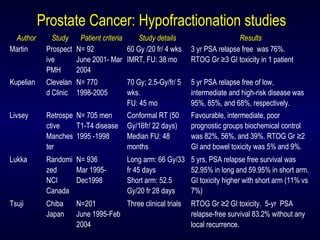
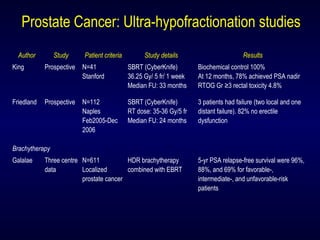
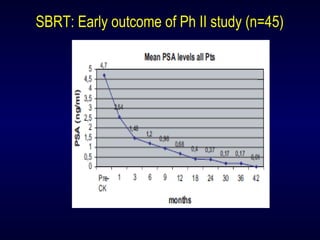
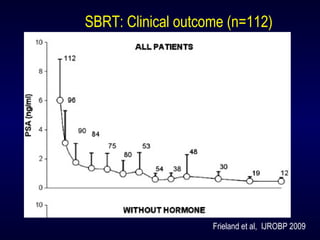
- Large prospective studies with over 500 patients and 5 years of follow up have shown that CyberKnife is as effective as long course radiation therapy for localized prostate cancer.
- SBRT/CyberKnife is now the standard of care treatment for localized prostate cancer.
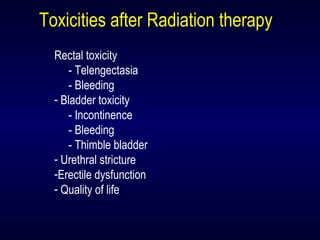
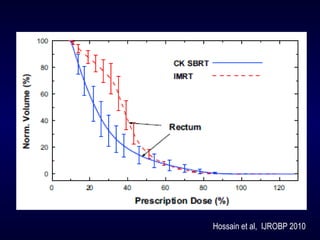
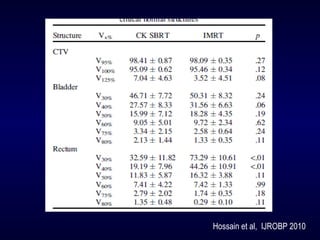
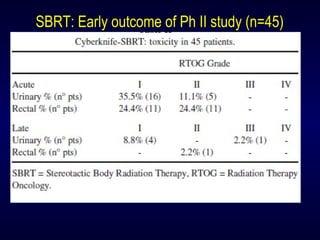
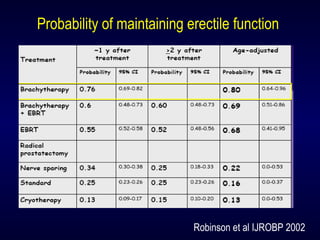
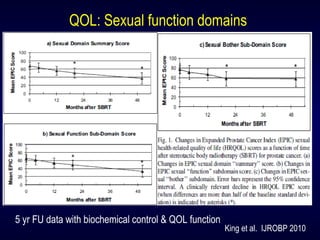
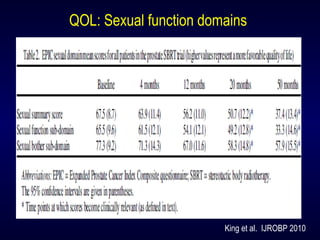
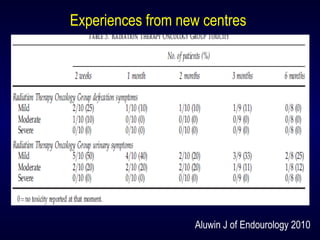
- Outcomes from CyberKnife treatment are similar to long course radiation therapy but side effects are less than 1% for prostate cancer.
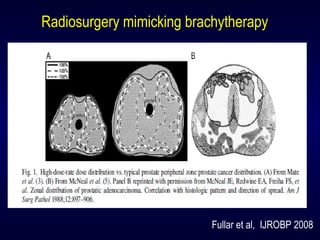
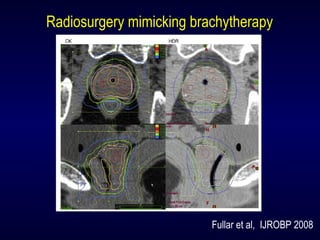
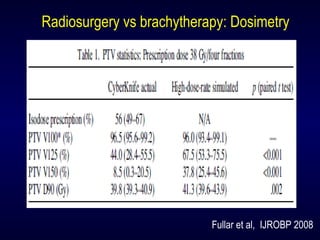
- CyberKnife provides a safe, outpatient treatment option in both primary and metastatic disease using short treatment courses and high radiation doses that can be effective for radioresistant diseases.