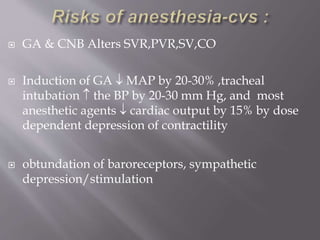
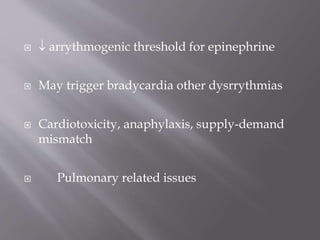
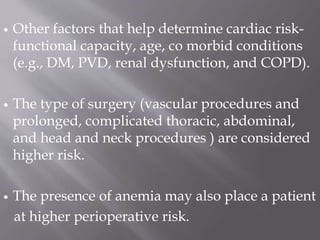
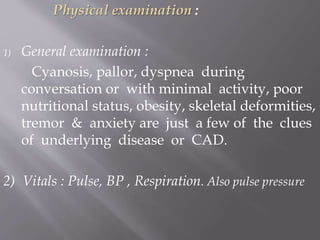
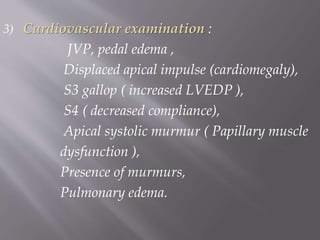
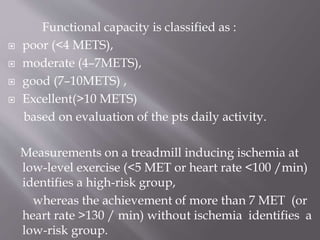
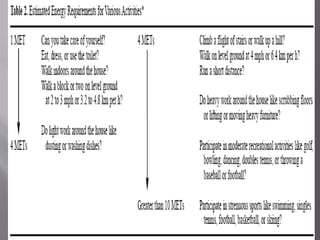
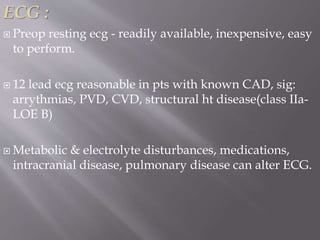
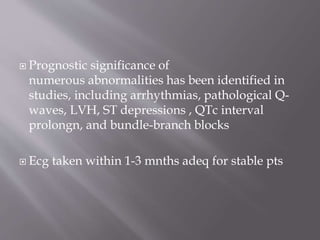
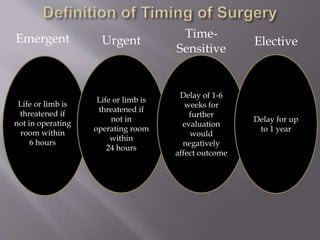
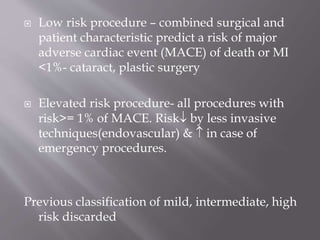
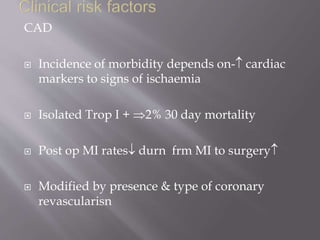
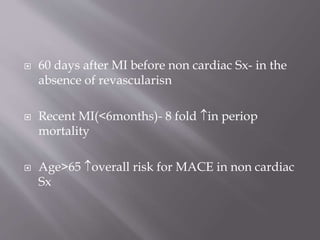
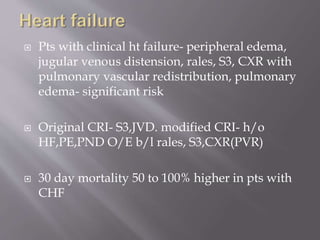
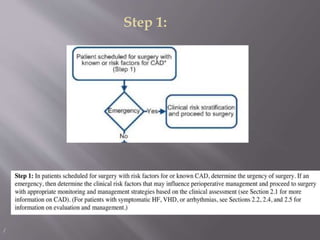
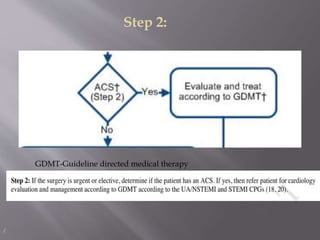
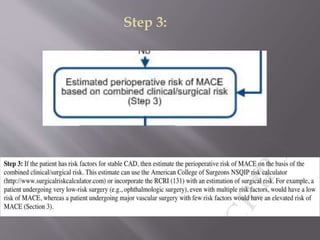
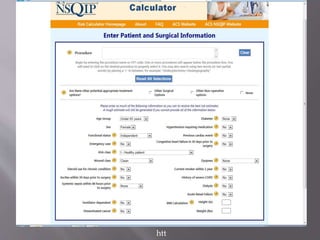
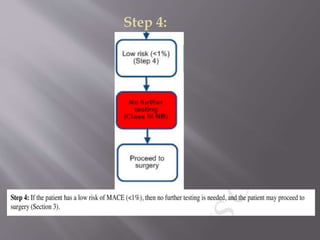
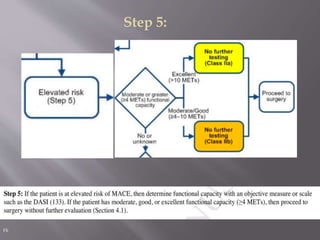
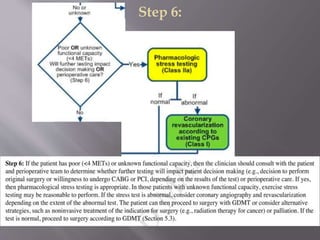
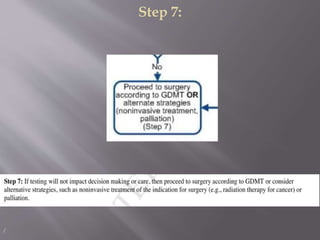
Dr. Brijesh Savidhan discusses strategies for evaluating cardiac risk in patients undergoing non-cardiac surgery. The goals are to identify patients at risk, evaluate the severity of underlying heart disease, and stratify surgical risk. A thorough history, physical exam, electrocardiogram, and assessment of functional capacity are recommended. For higher-risk patients, stress testing and evaluation of left ventricular function may be considered to guide management and minimize perioperative complications. Overall, a multidisciplinary approach is important to optimize cardiac status, determine the safest location and timing of surgery, and develop an anesthesia plan tailored to each patient's cardiac condition.