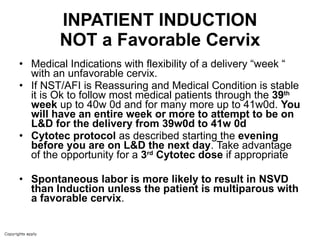
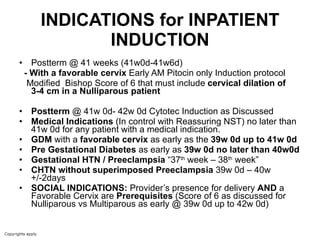
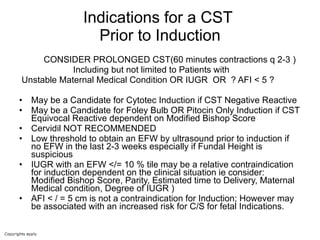
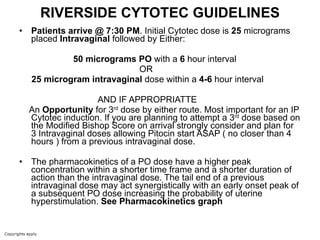
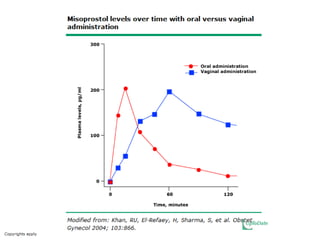
The document provides guidelines for cervical ripening and labor induction. Key points include:
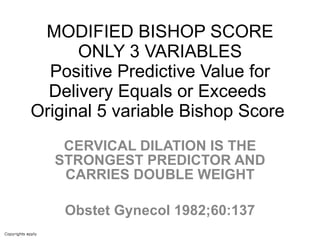
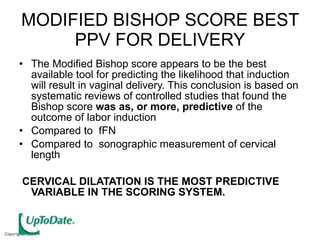
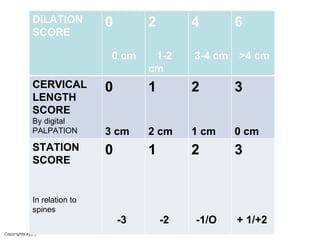
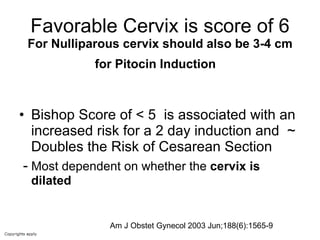
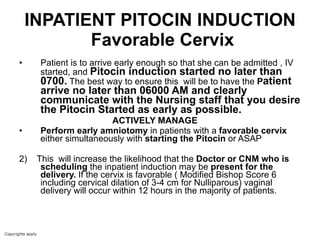
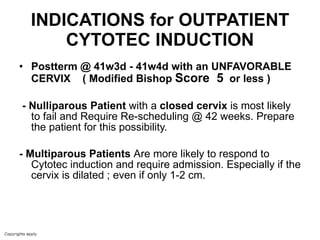
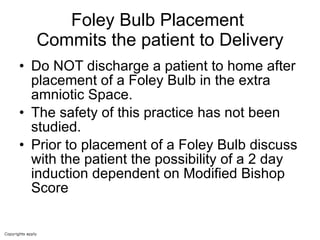
- The modified Bishop score is the best tool for predicting successful induction outcomes. Cervical dilation carries the most weight.
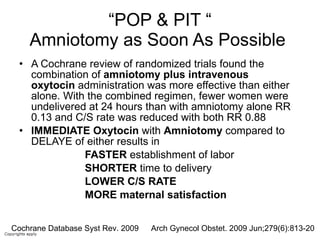
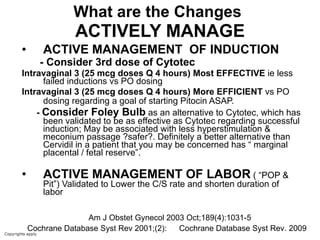
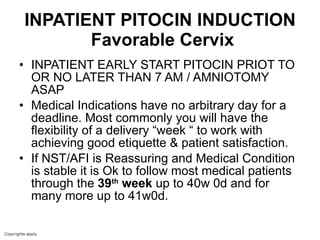
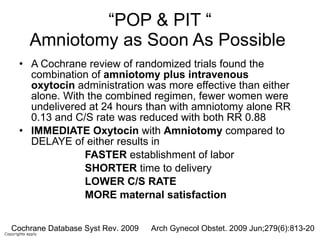
- Early amniotomy and oxytocin ("pop and pit") results in faster labor onset, shorter delivery time, and lower C-section rates compared to delayed amniotomy or oxytocin alone.
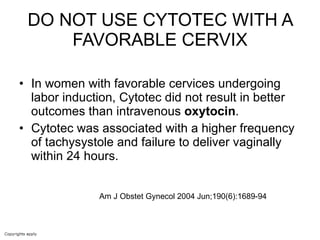
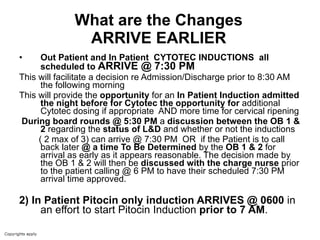
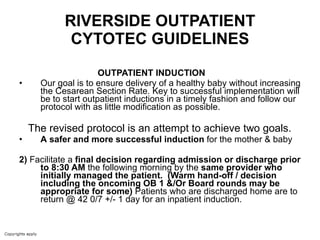
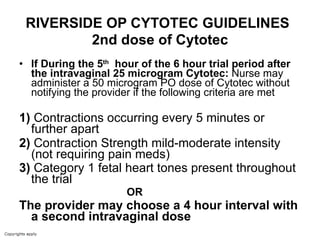
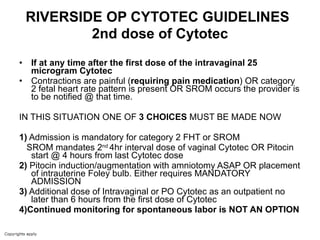
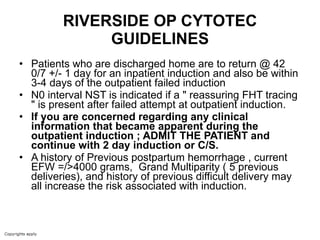
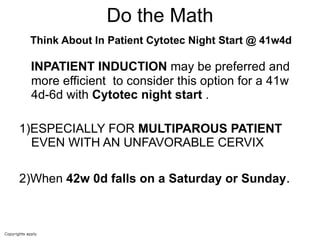
- Outpatient cervical ripening with misoprostol (Cytotec) should allow assessment for admission or discharge by 8:30am following the induction attempt.