This document defines growth and development and how they are assessed in children. It discusses:
- Growth is an increase in size due to cell multiplication and protein/DNA content, while development refers to functional/physiological maturation.
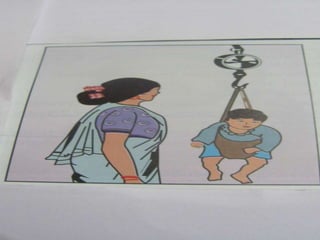
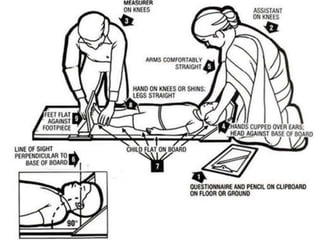
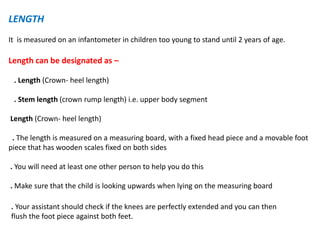
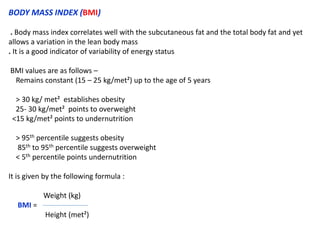
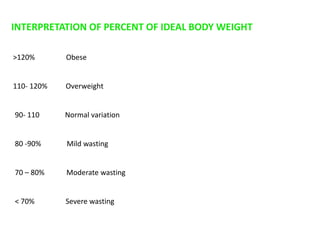
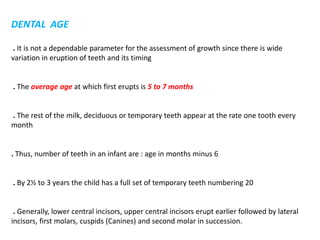
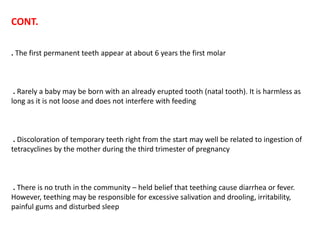
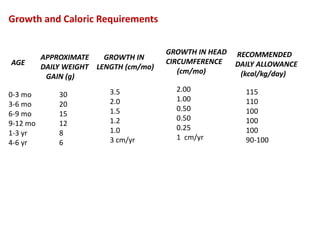
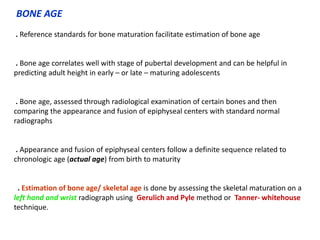
- Growth can be measured through physical anthropometry of weight, length/height, head circumference, chest circumference, mid-arm circumference, and bone age assessed on X-rays.
- Factors like genetics, nutrition, socioeconomics, environment, and chronic diseases influence a child's growth and development. Growth and development begin at conception and continue until maturity.