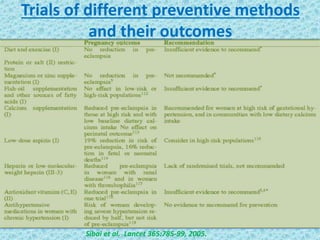
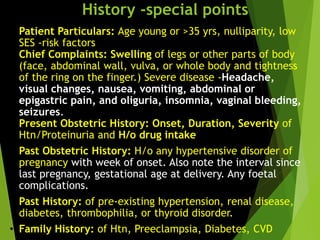
This document discusses hypertensive disorders in pregnancy, including gestational hypertension and preeclampsia. Some key points:
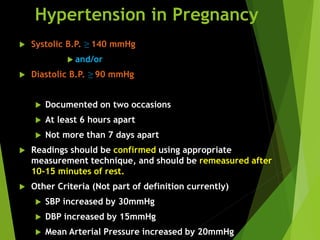
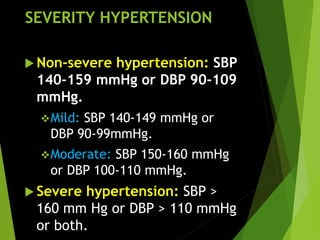
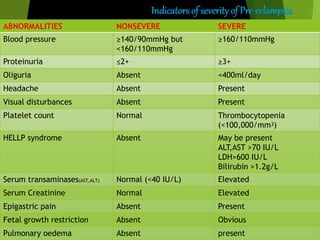
- Gestational hypertension is defined as new hypertension after 20 weeks without proteinuria, resolving postpartum. It affects 5-10% of pregnancies and can progress to preeclampsia in 15-25% of cases.
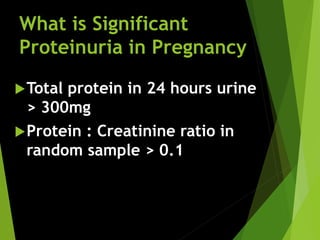
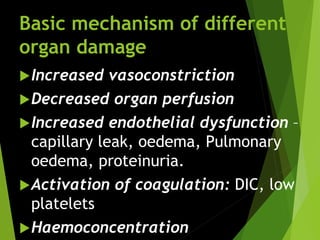
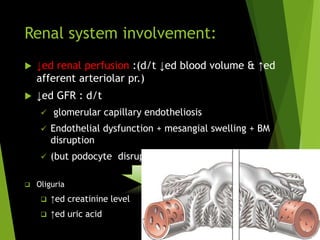
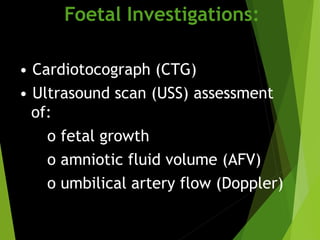
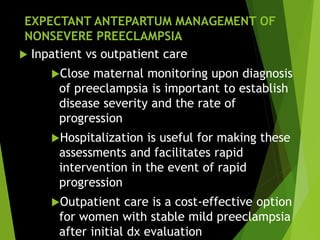
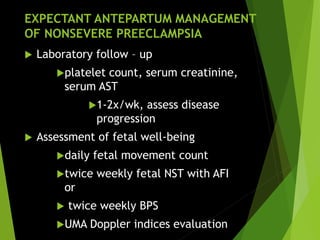
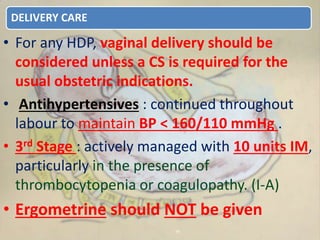
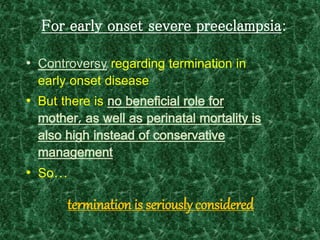
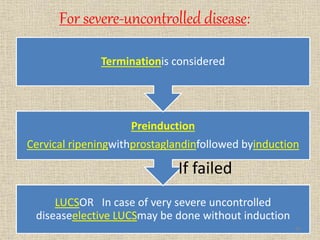
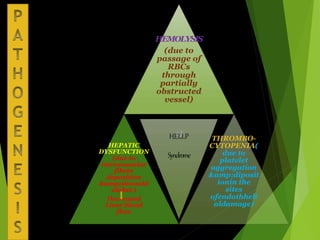
- Preeclampsia is defined as new hypertension and proteinuria after 20 weeks, resolving postpartum. It is associated with severe maternal complications and is a leading cause of preterm birth and intrauterine growth restriction.
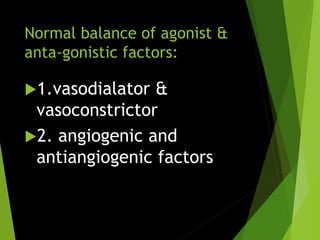
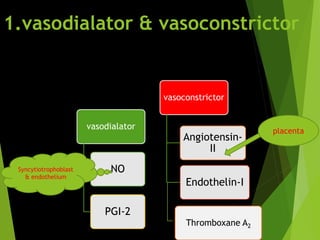
- Both conditions are thought to involve reduced placental implantation in early pregnancy followed by maternal symptoms in later pregnancy due to factors