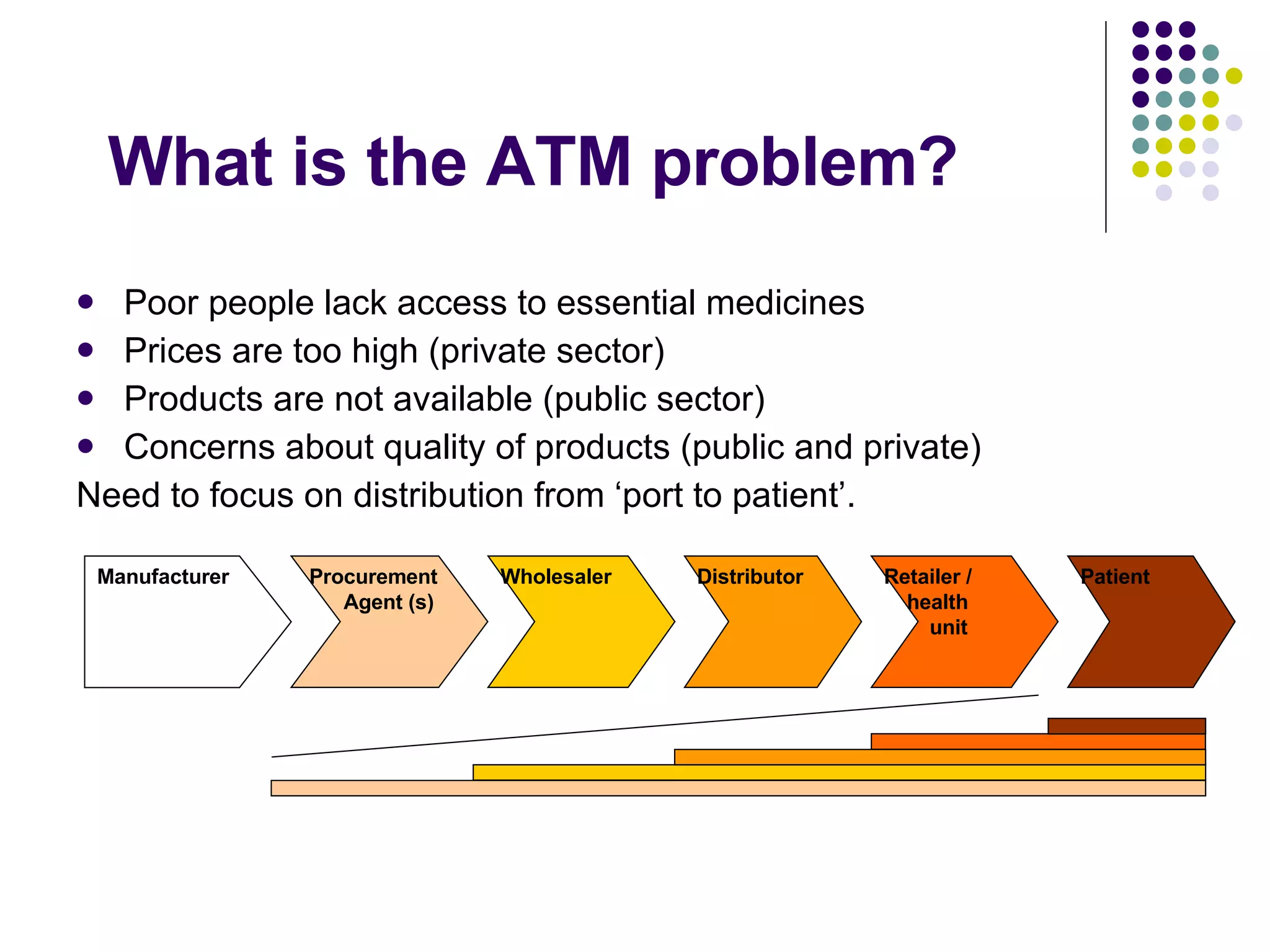
The document outlines the challenges of access to essential medicines in Ghana, focusing on the need for governance, transparency, and accountability within the pharmaceutical supply chain. It highlights the roles of civil society organizations (CSOs) and media in enhancing public awareness and engagement while addressing issues such as pricing, quality, and availability of medicines. Proposed strategies include improved data collection, monitoring of medicines, and fostering stakeholder dialogue to develop a long-term plan for transparency and accountability in the health sector.