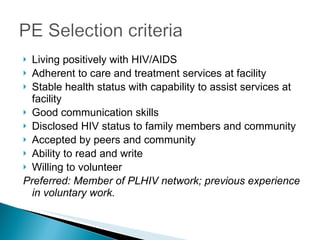
The document summarizes ICAP Tanzania's peer education program which aims to increase adherence and psychosocial support for people living with HIV. The program trains people living with HIV to serve as peer educators who provide counseling, health talks, and community outreach. Peer educators help 180 people across 35 sites and have established over 100 support groups. Evaluation found the program increased clients' adherence, reduced stigma, and improved tracing of patients lost to follow up. Challenges include a lack of health worker support and no formal policy to institutionalize the peer education role in health facilities.