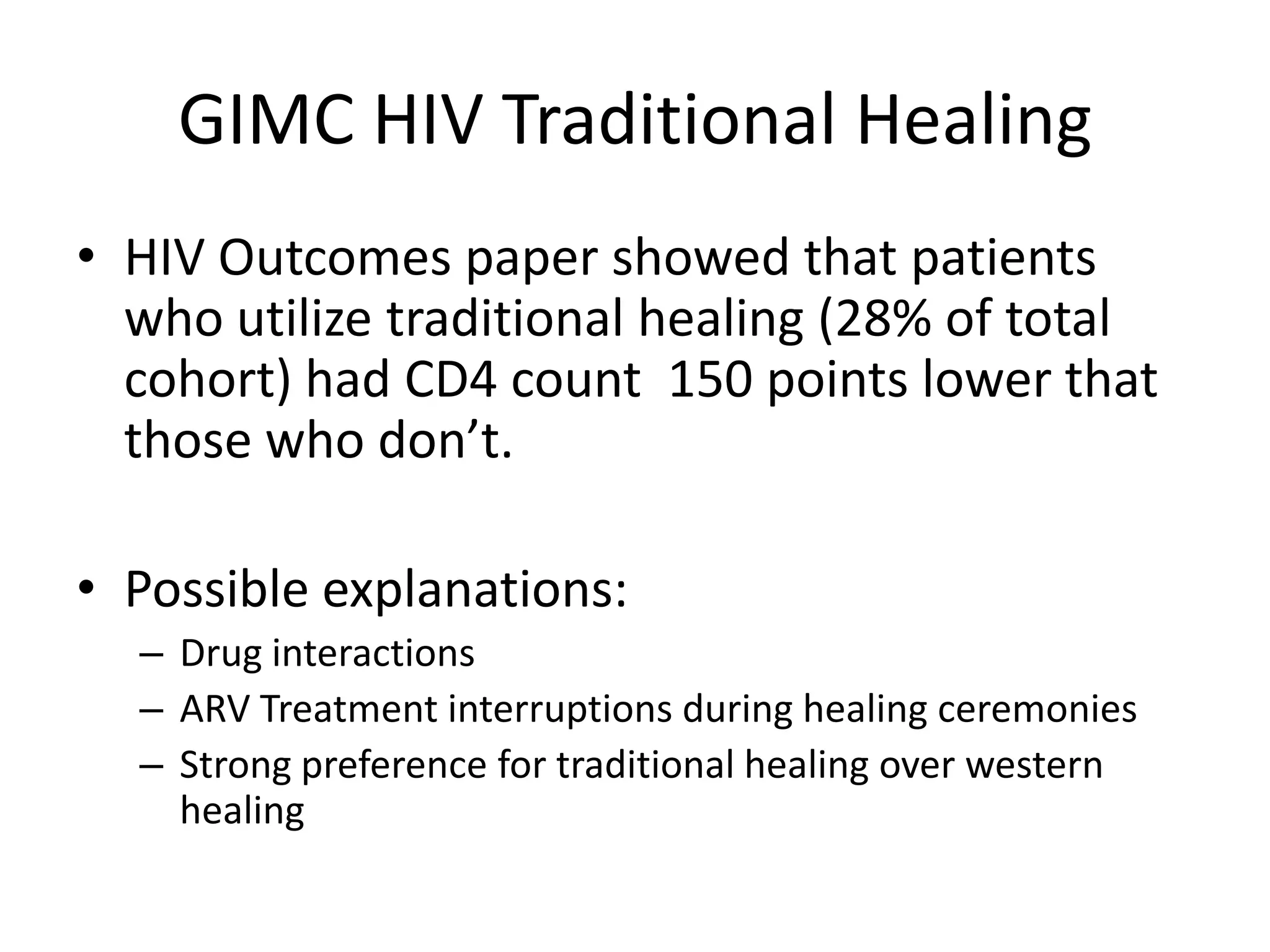
This document describes the case of a man diagnosed with HIV after multiple visits to an IHS clinic. It outlines the IHS HIV care team that successfully treated the patient's physical and mental health issues. This included pharmacists, physicians, a nurse specialist, nutritionist, and traditional healer. The care team works to improve HIV screening, treatment, and destigmatize HIV in American Indian communities.