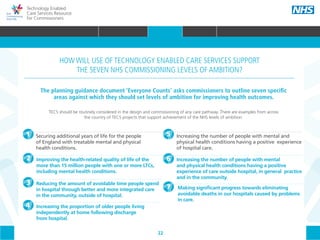
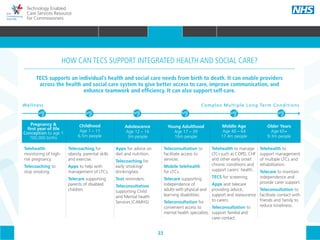
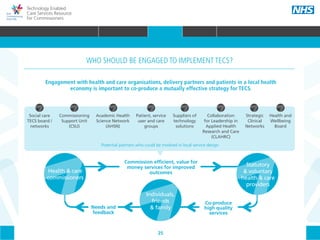
This document provides an overview of the policy context relevant to technology enabled care services (TECS). It discusses key frameworks and initiatives that aim to improve health and social care outcomes through greater integration and personalization of services. TECS can help achieve the goals of these policies by supporting self-care, coordinating services, and empowering patients. The document outlines how TECS relates to priorities around long-term conditions, new models of primary care, integrated health and social care, and personal health budgets.