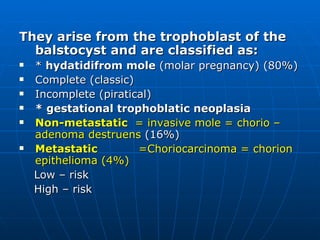
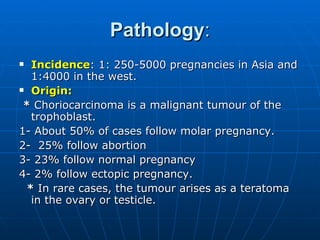
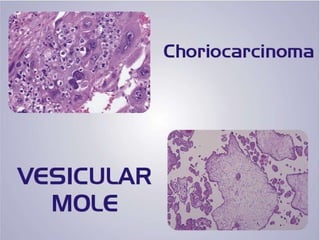
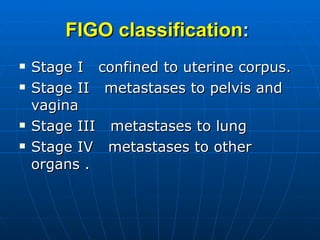
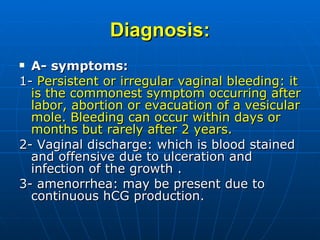
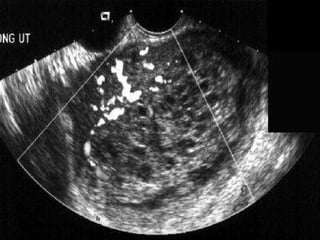
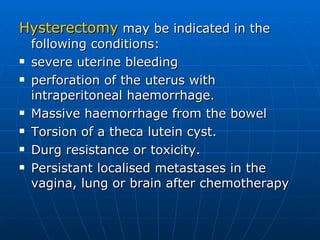
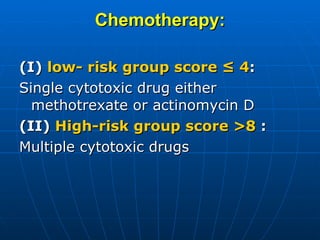
Gestational trophoblastic diseases arise from the trophoblast and include hydatidiform moles (80%), gestational trophoblastic neoplasia (16%), and choriocarcinoma (4%). Choriocarcinoma is a malignant tumor of the trophoblast that most commonly spreads to the lungs (80%) and vagina (30%). Diagnosis involves symptoms of bleeding, hCG levels, imaging and biopsy. Treatment is usually chemotherapy, with hysterectomy as an option for resistant cases.