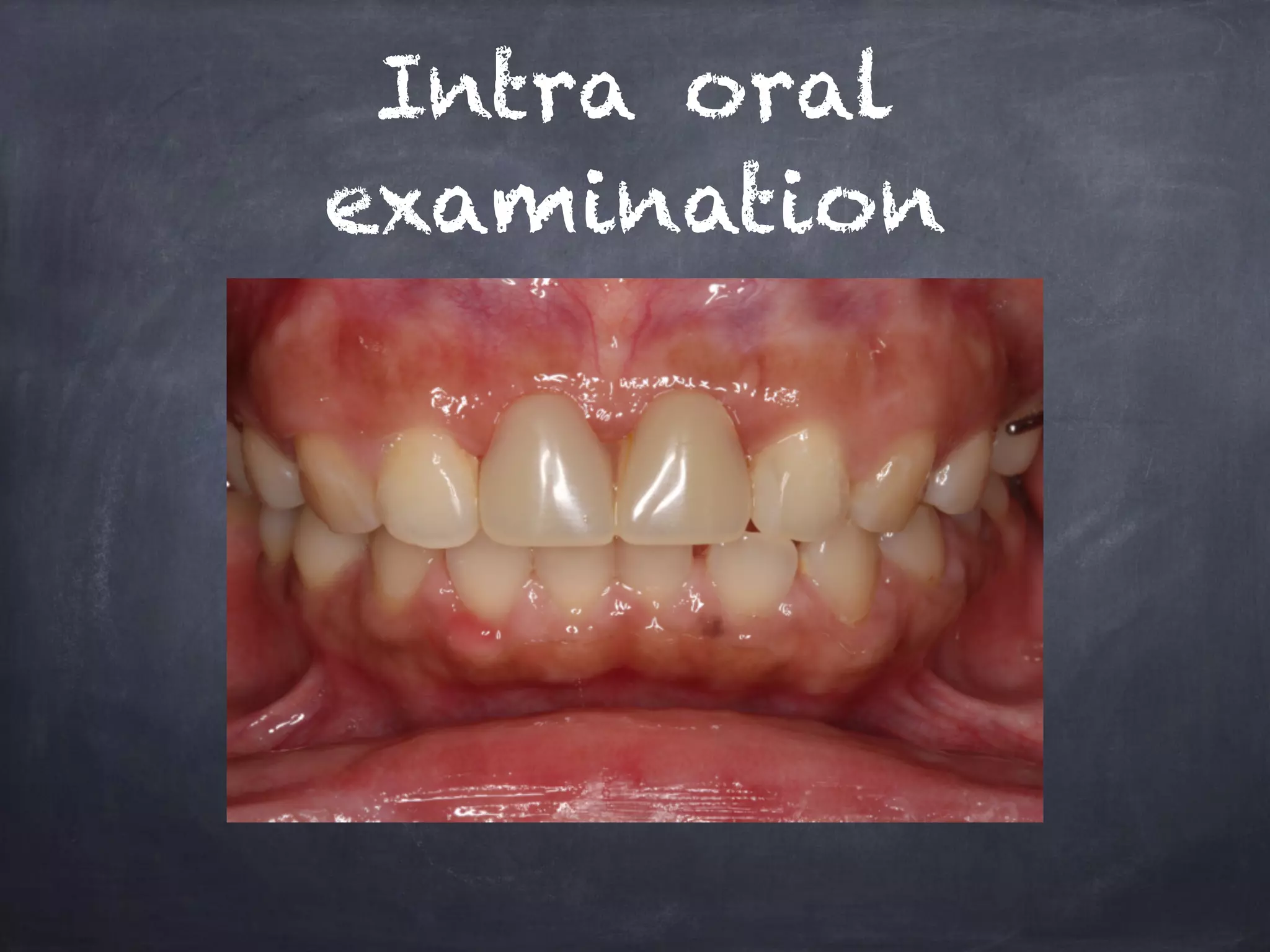
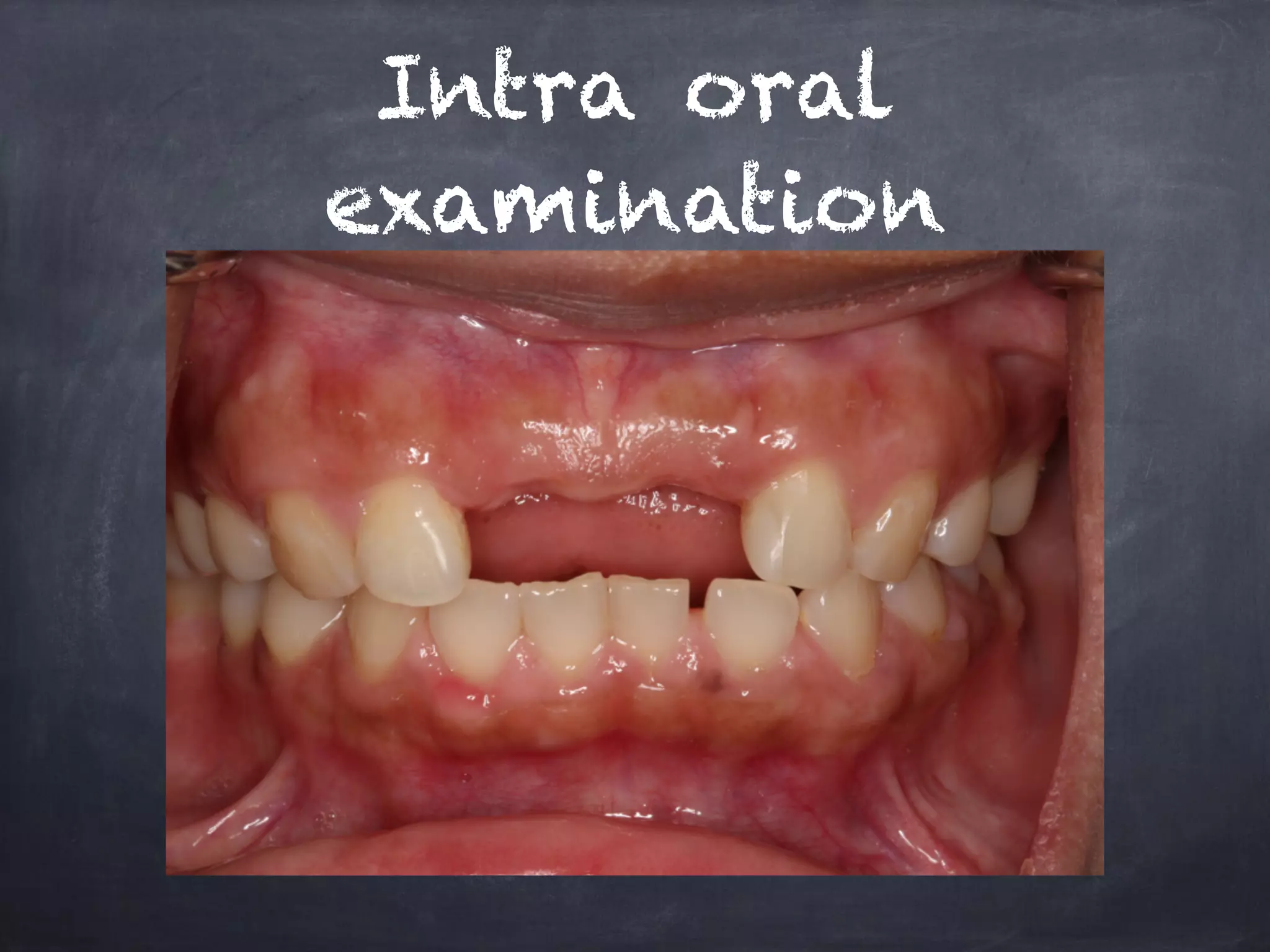
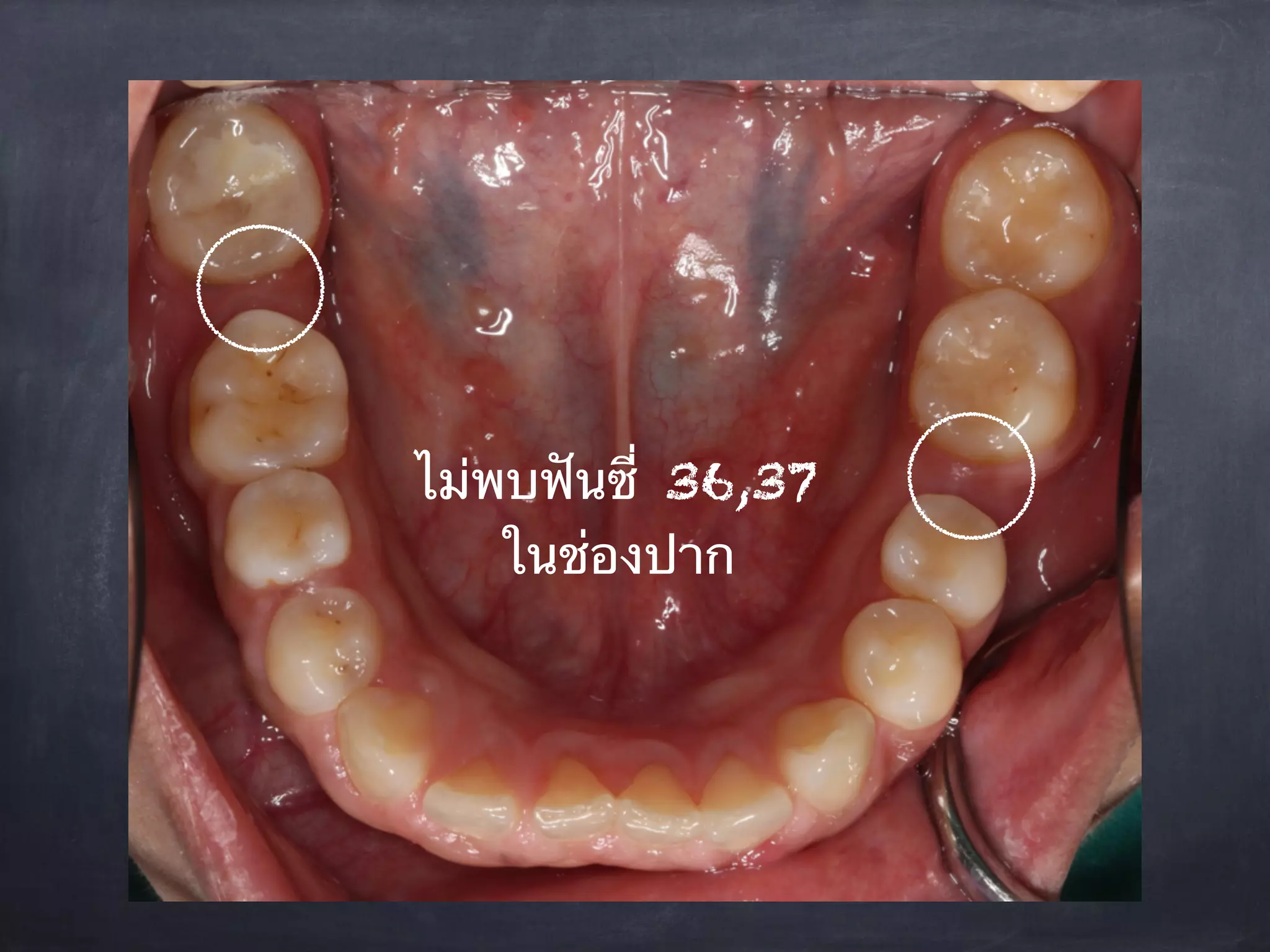
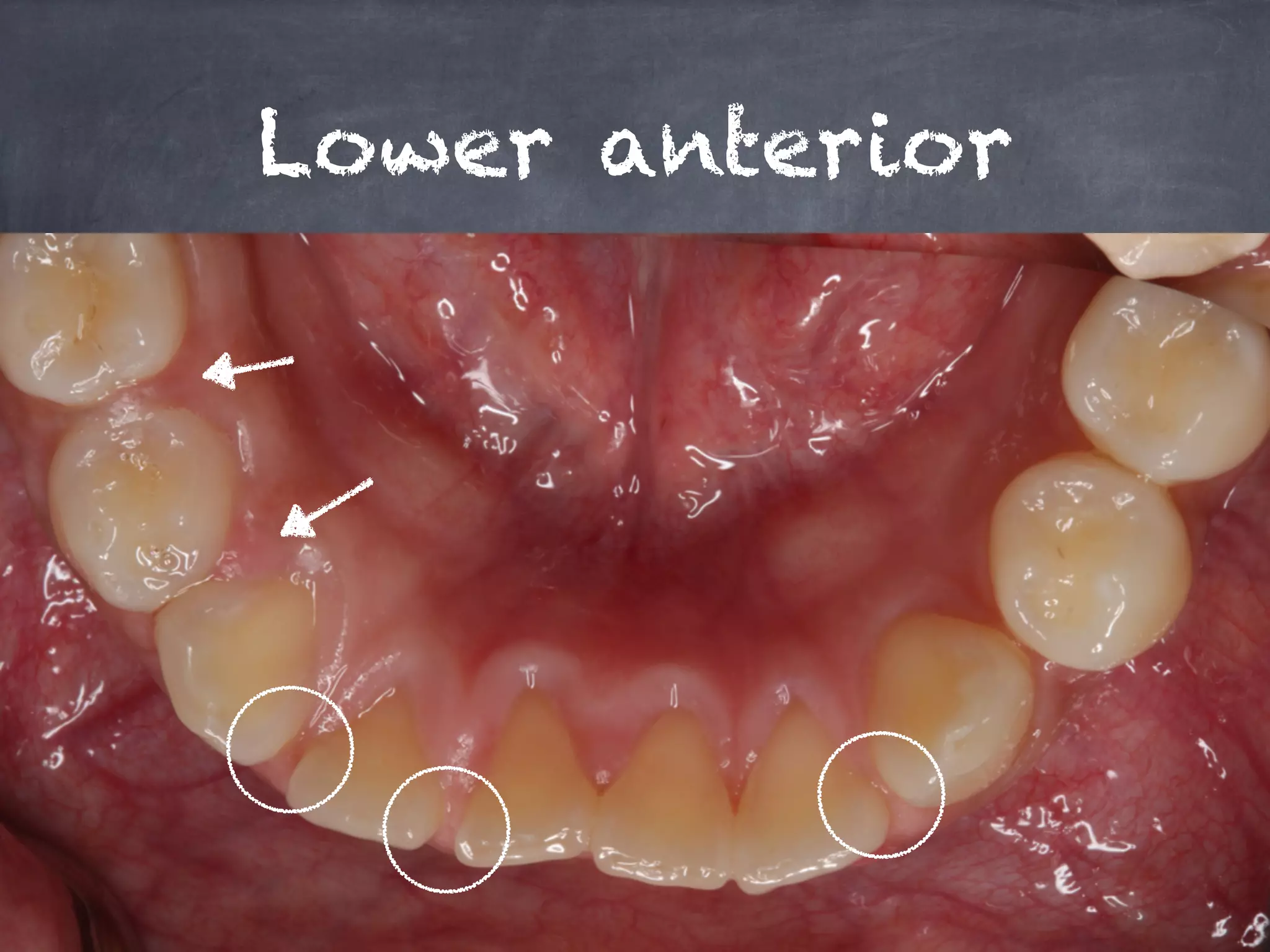
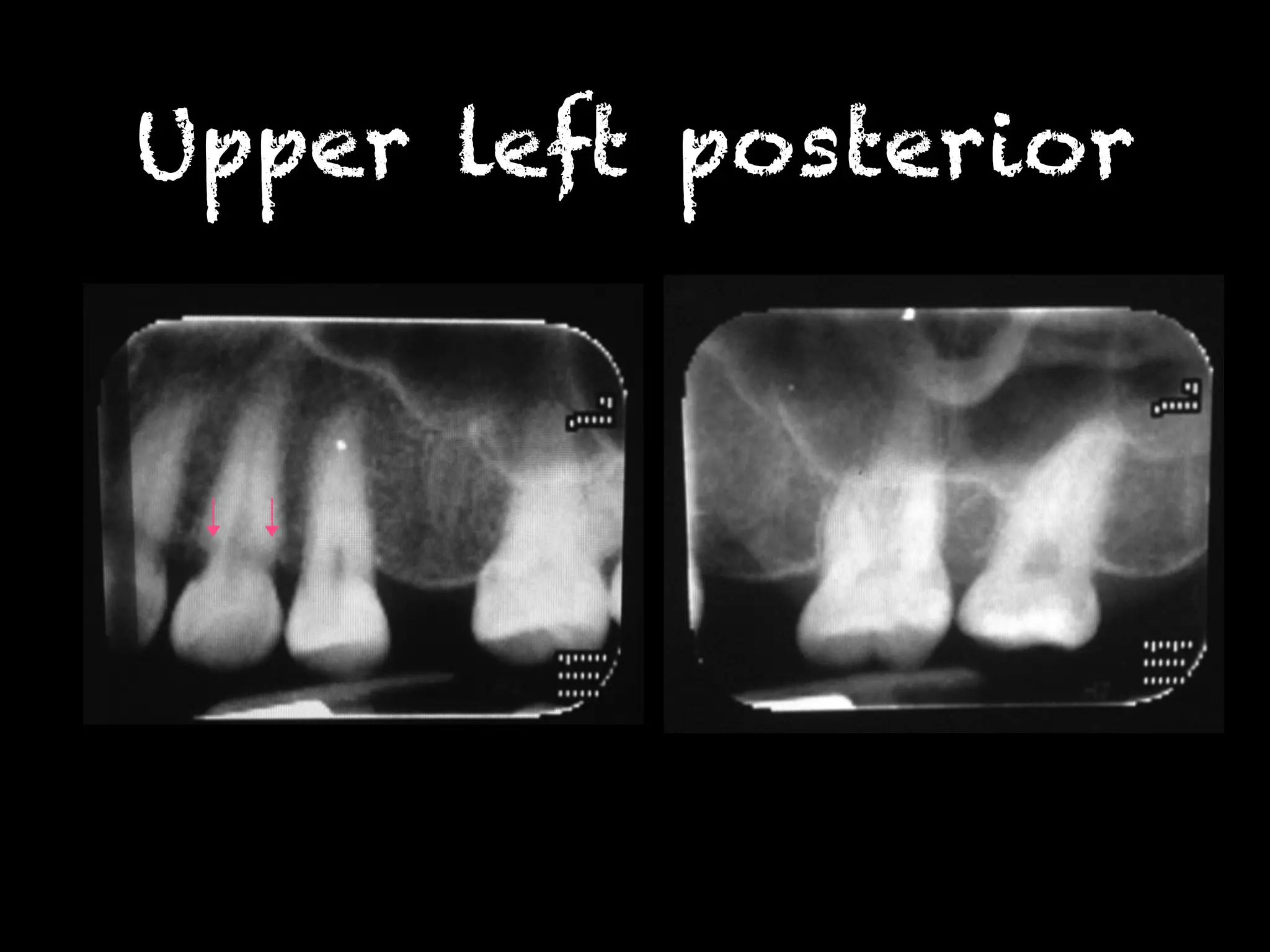
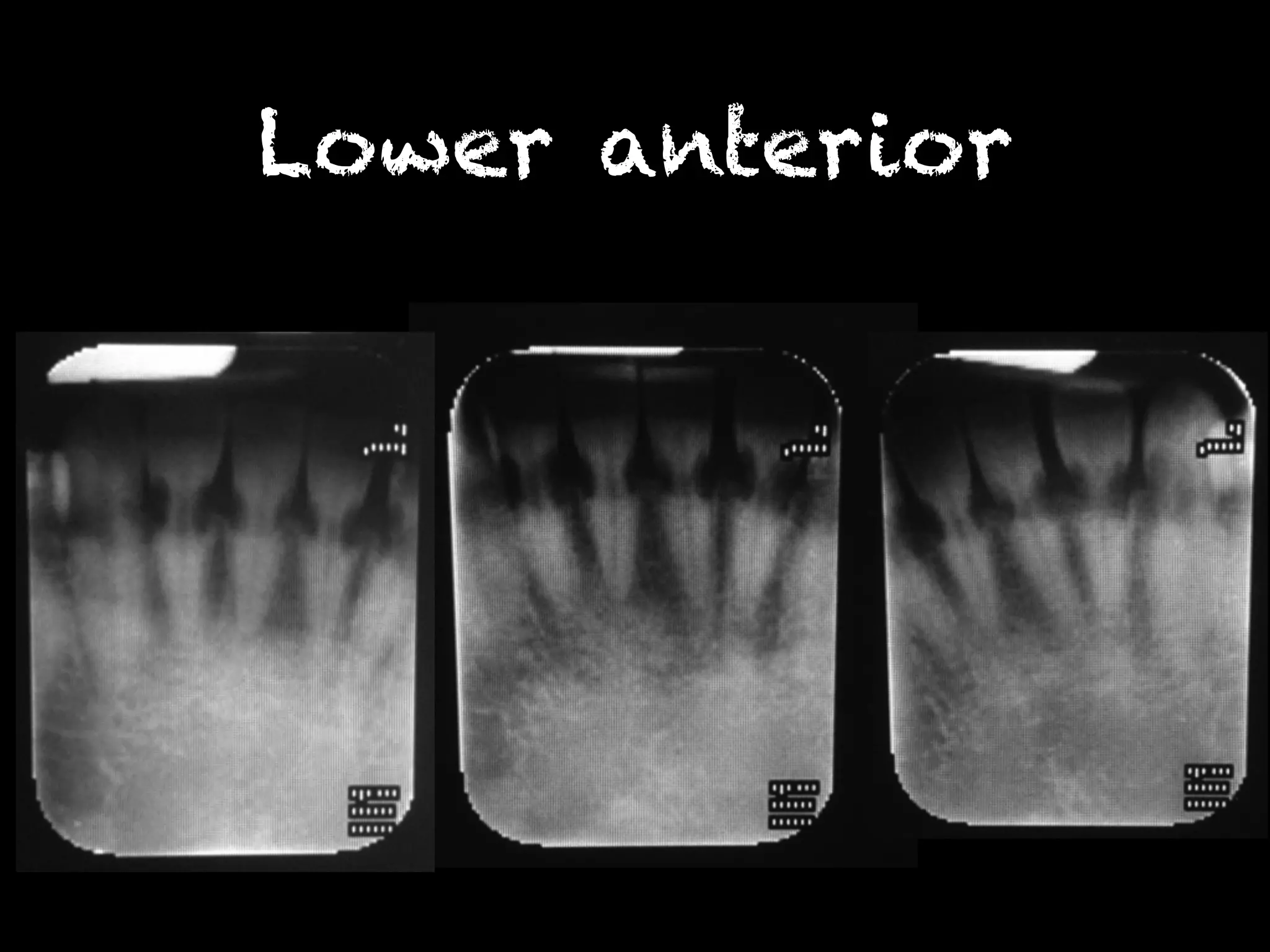
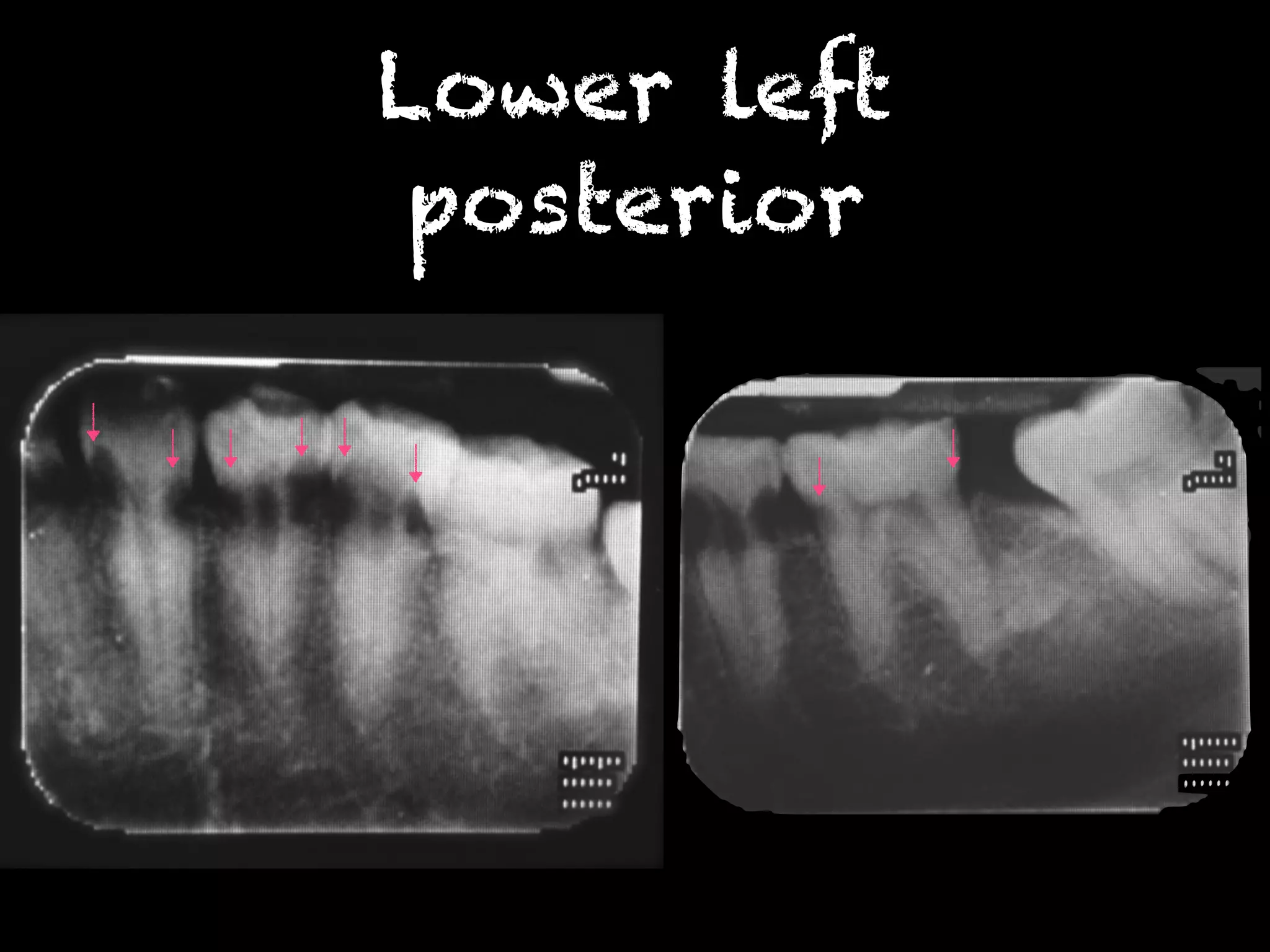
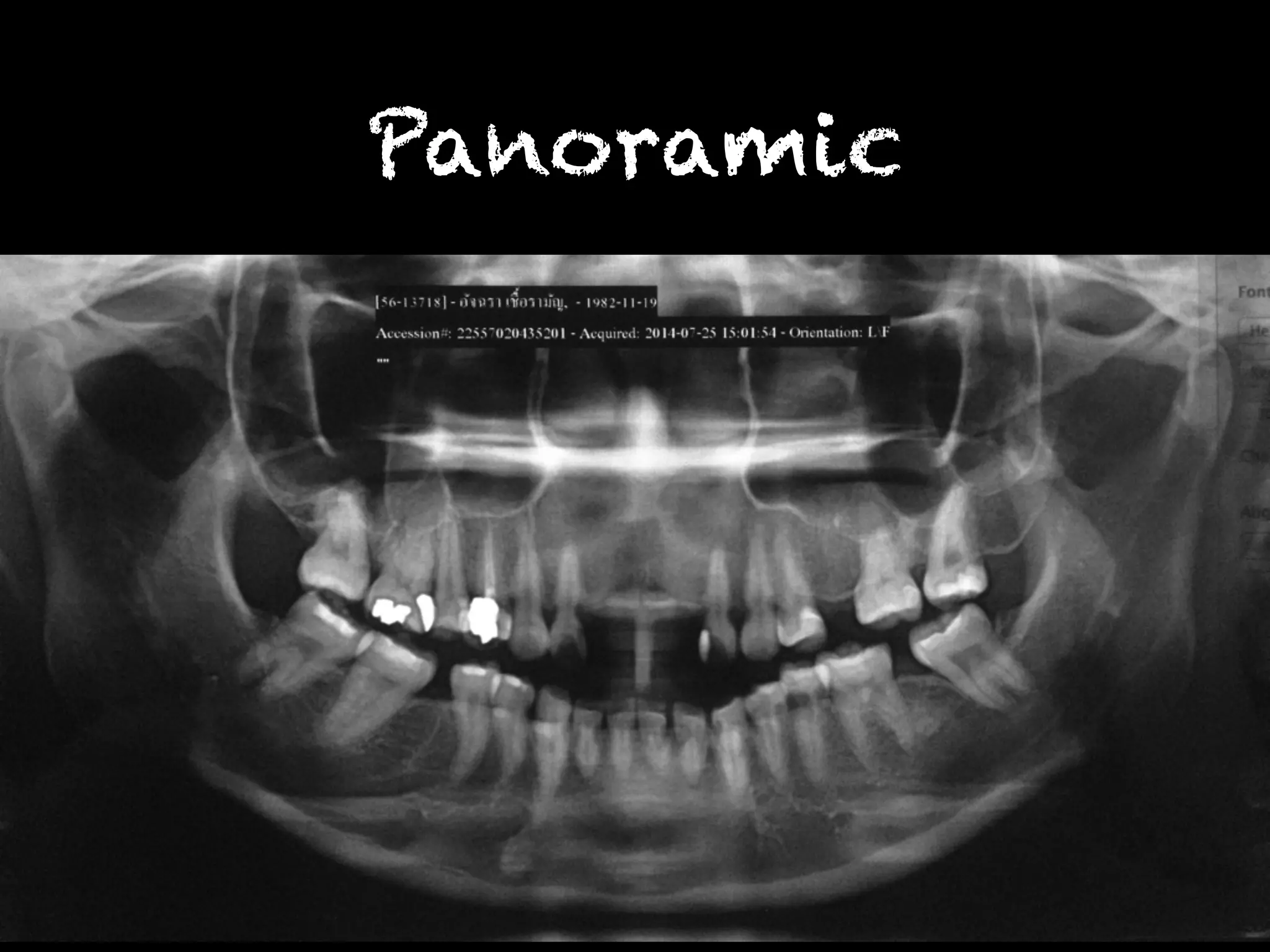
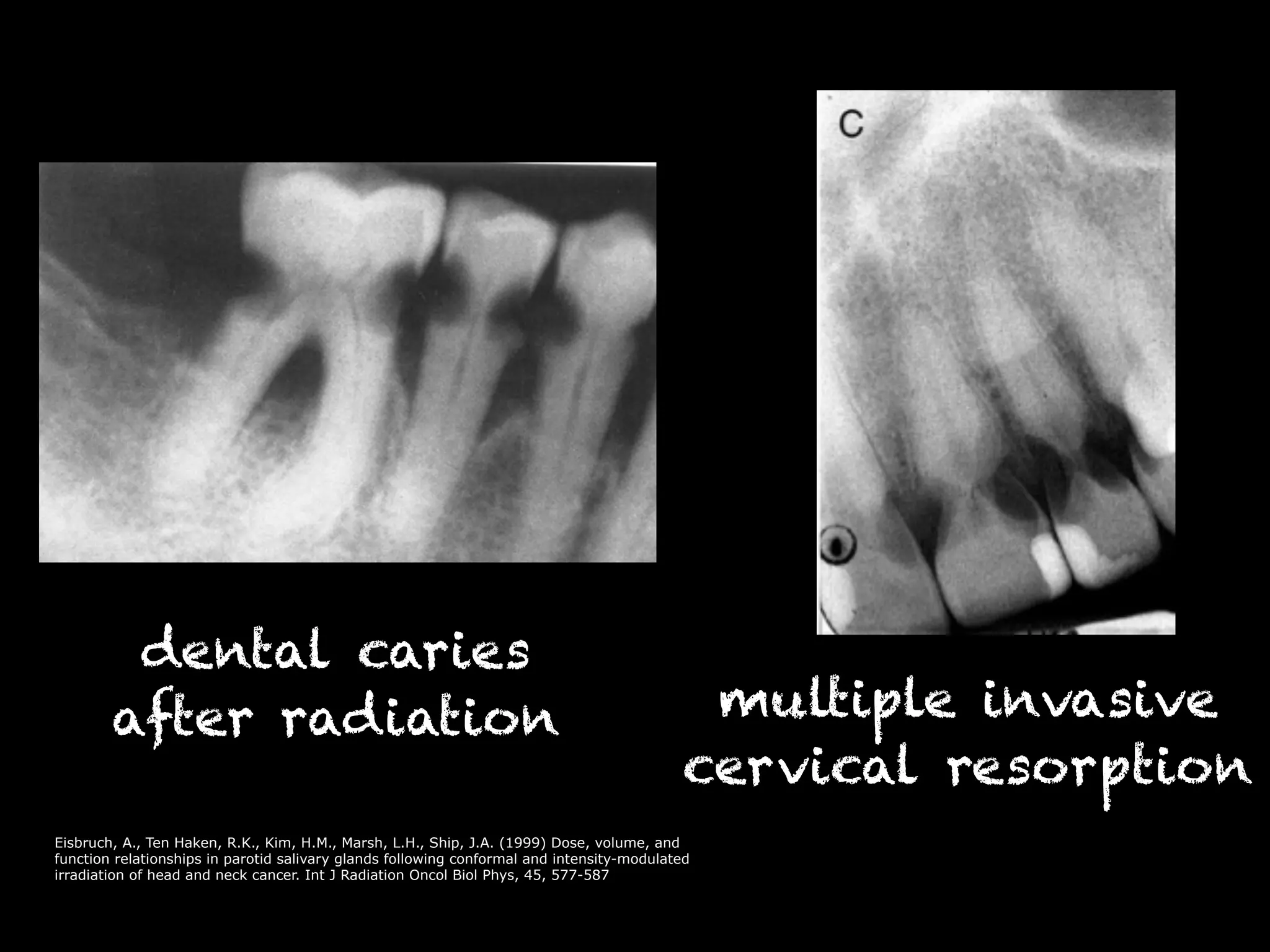
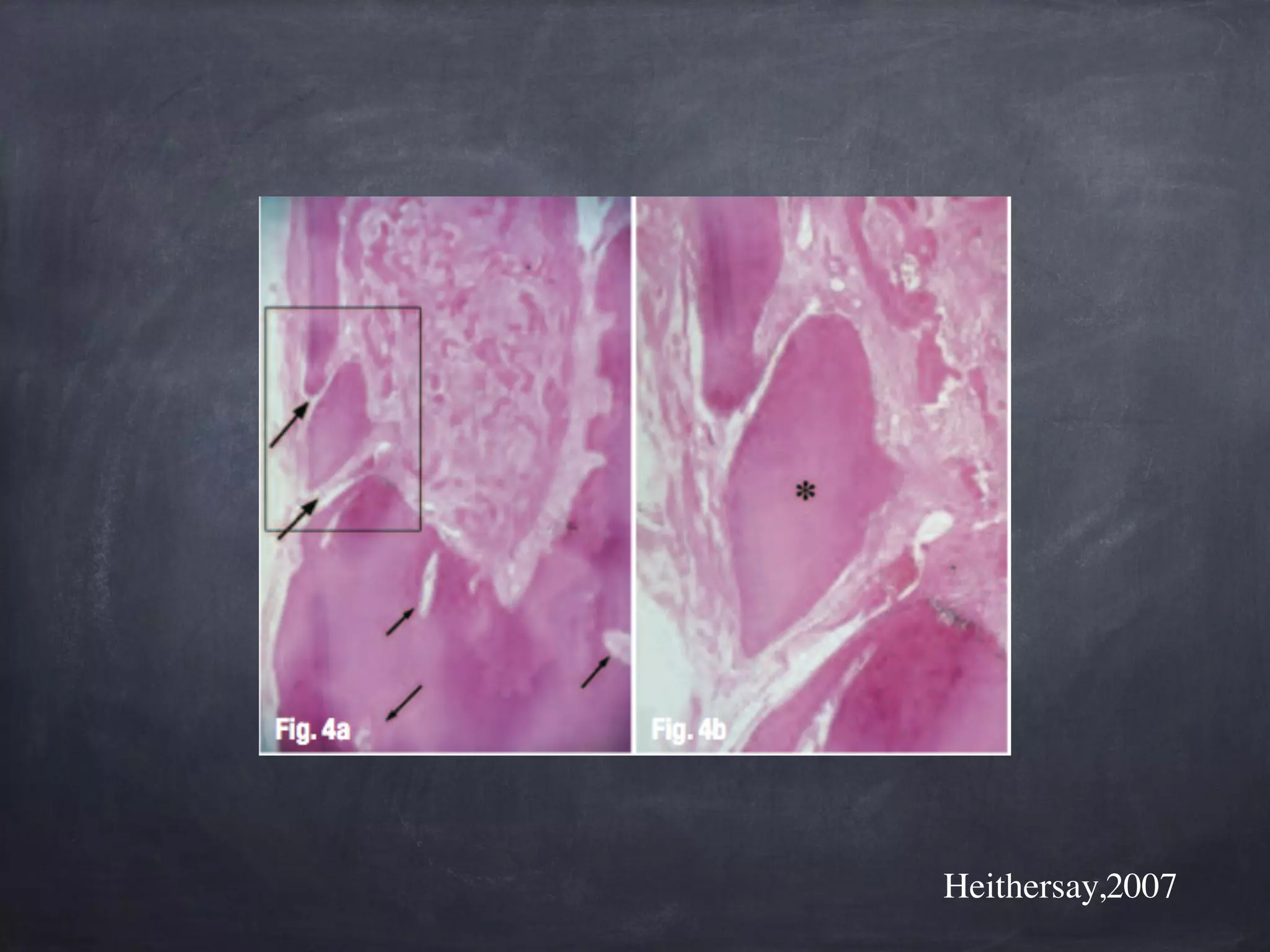
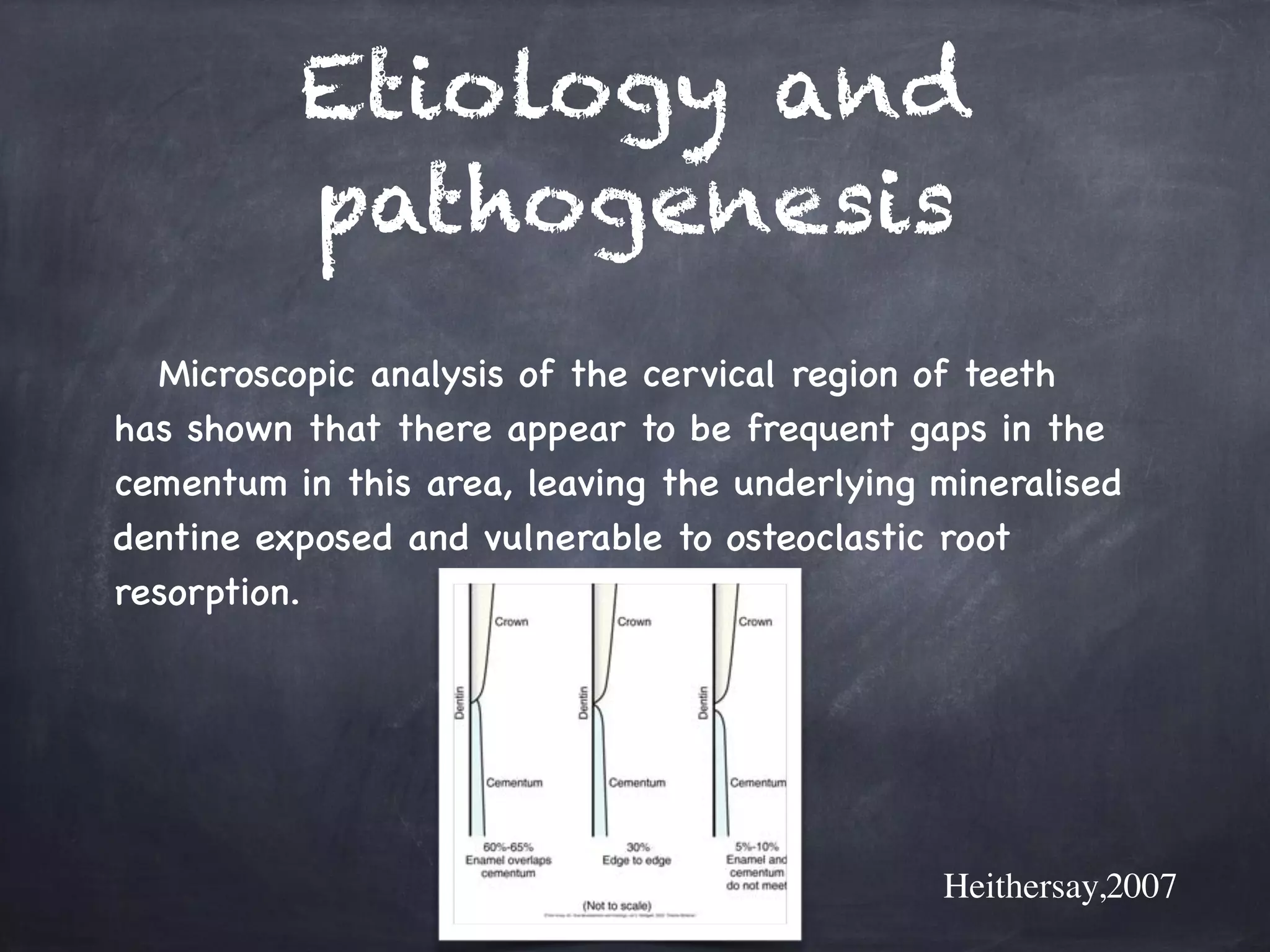
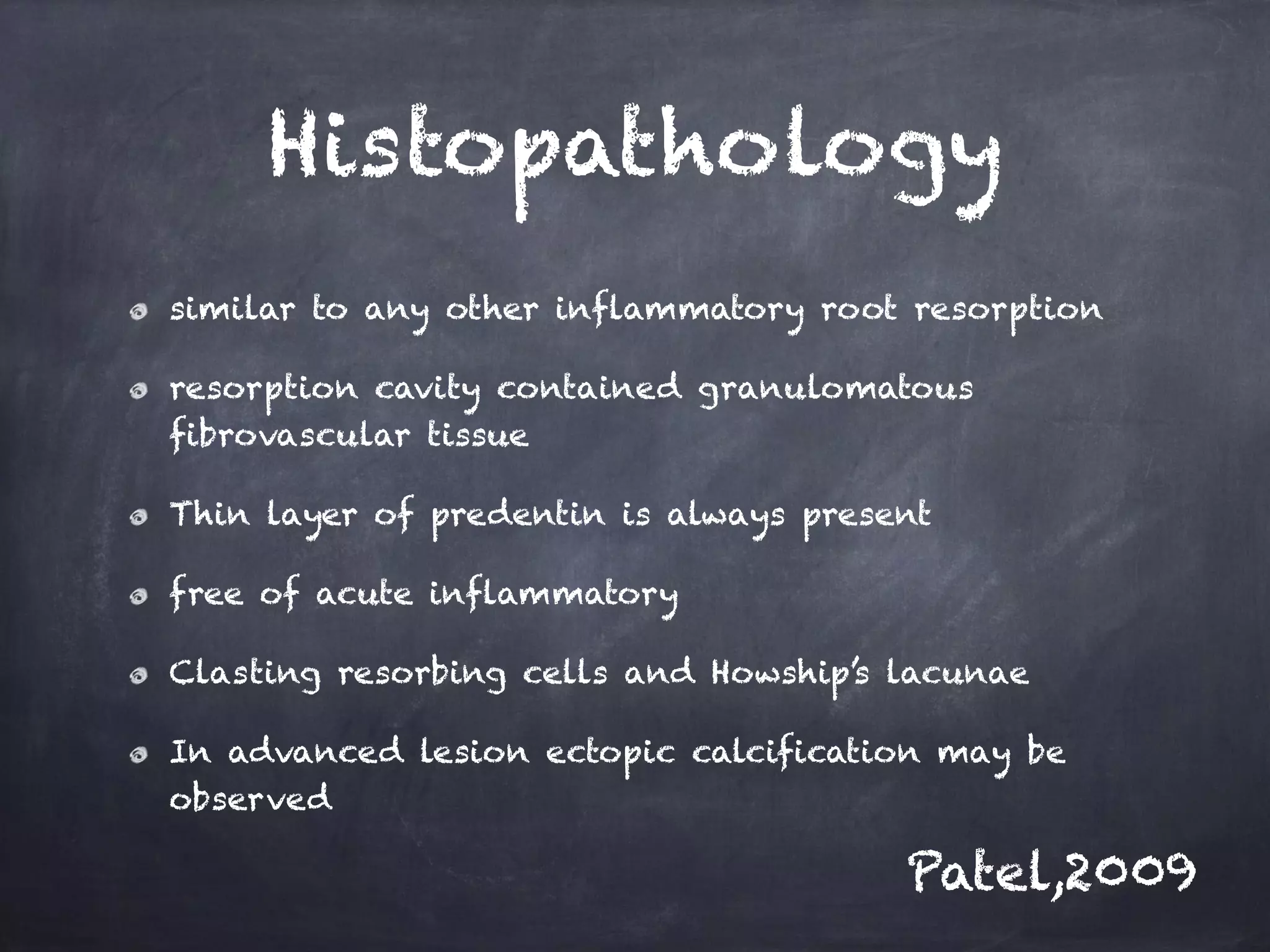
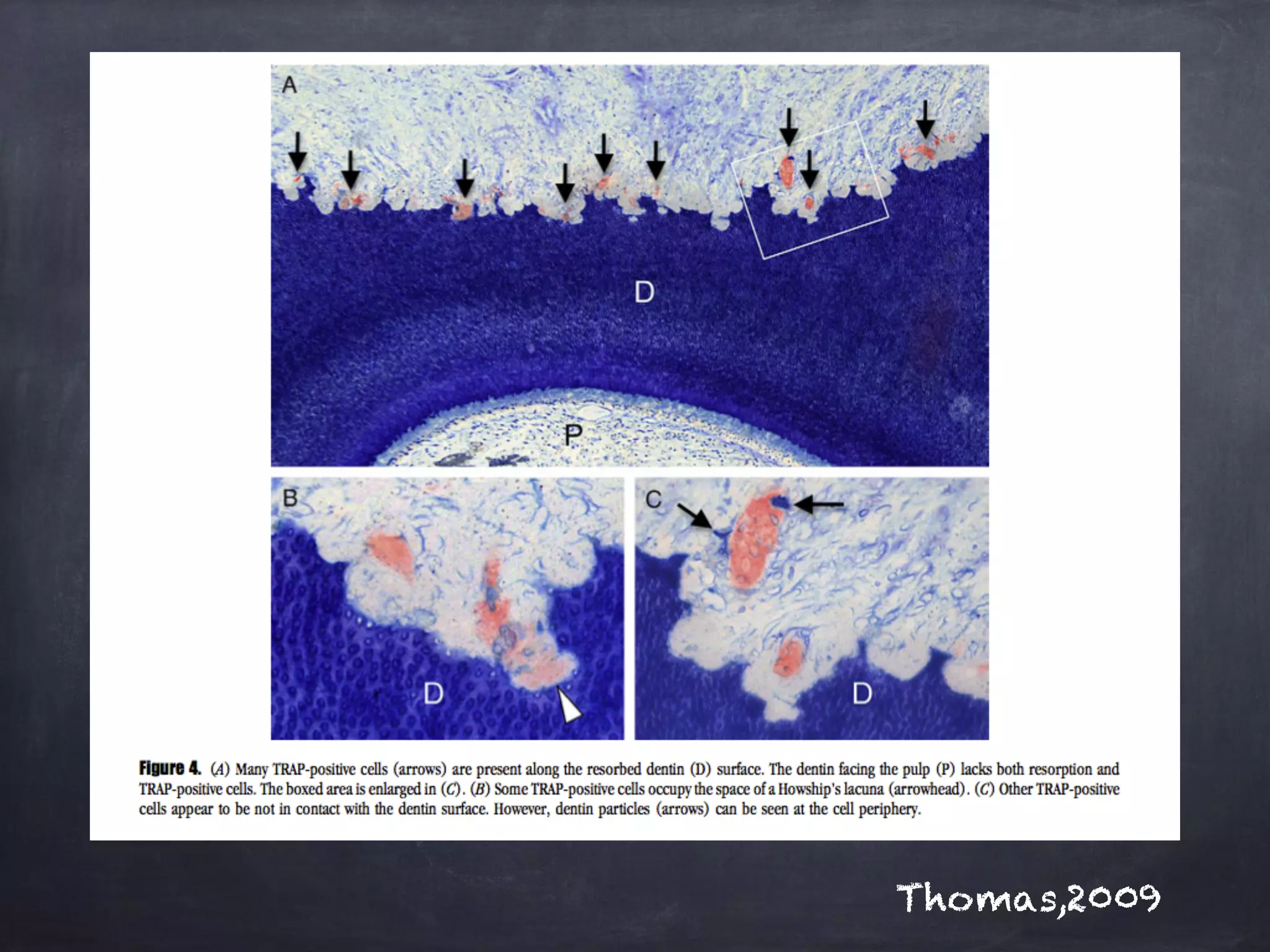
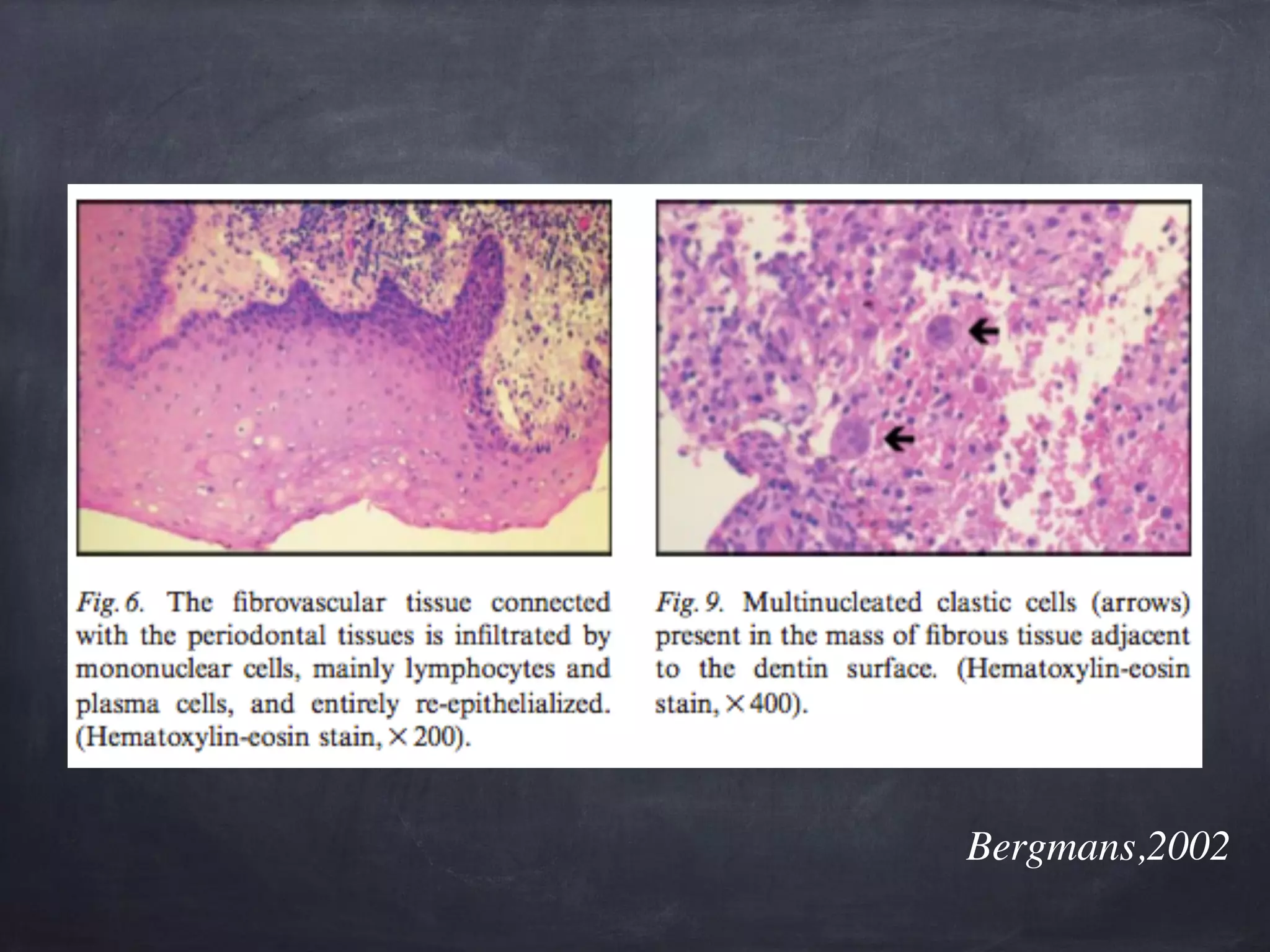
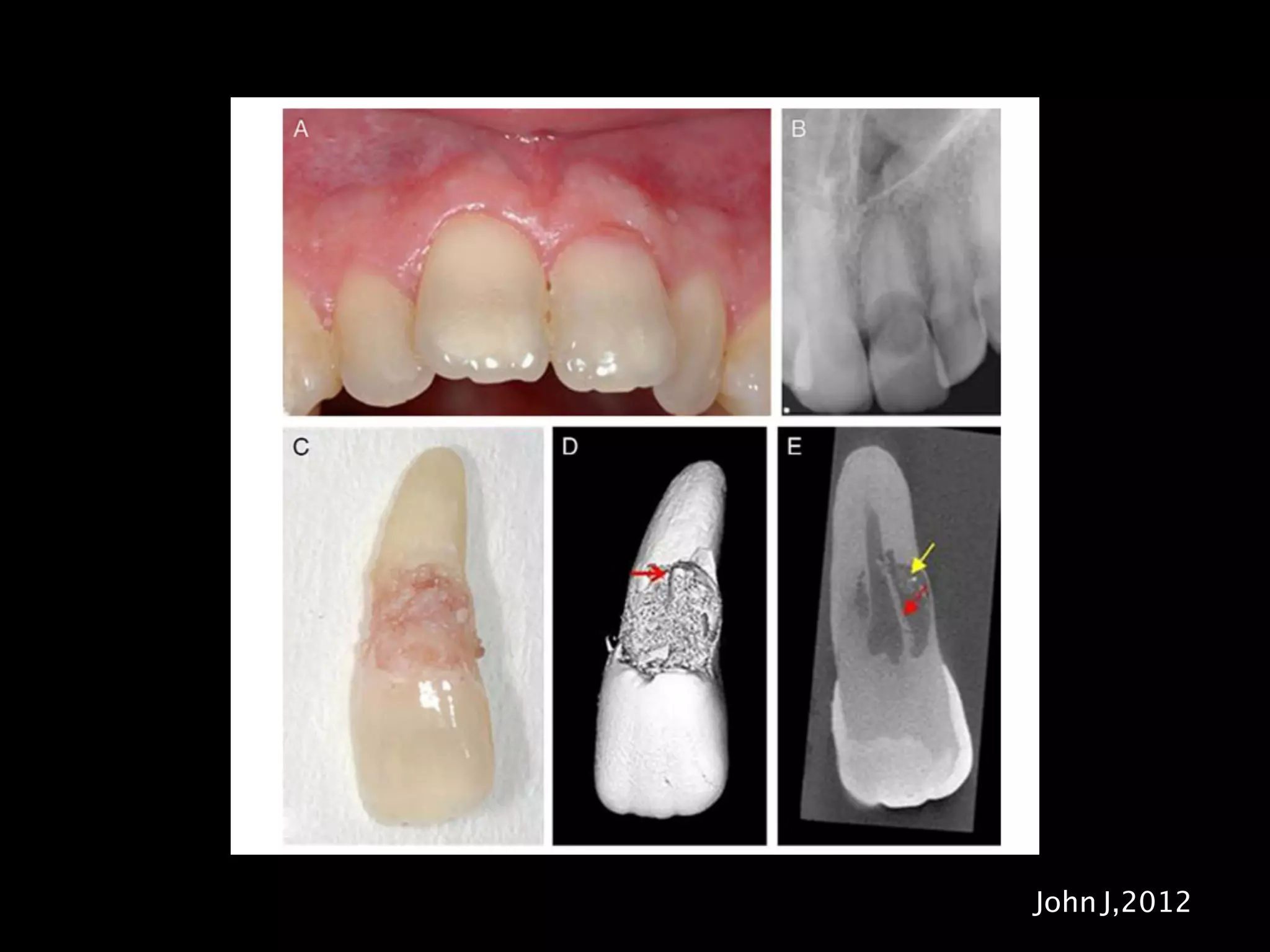
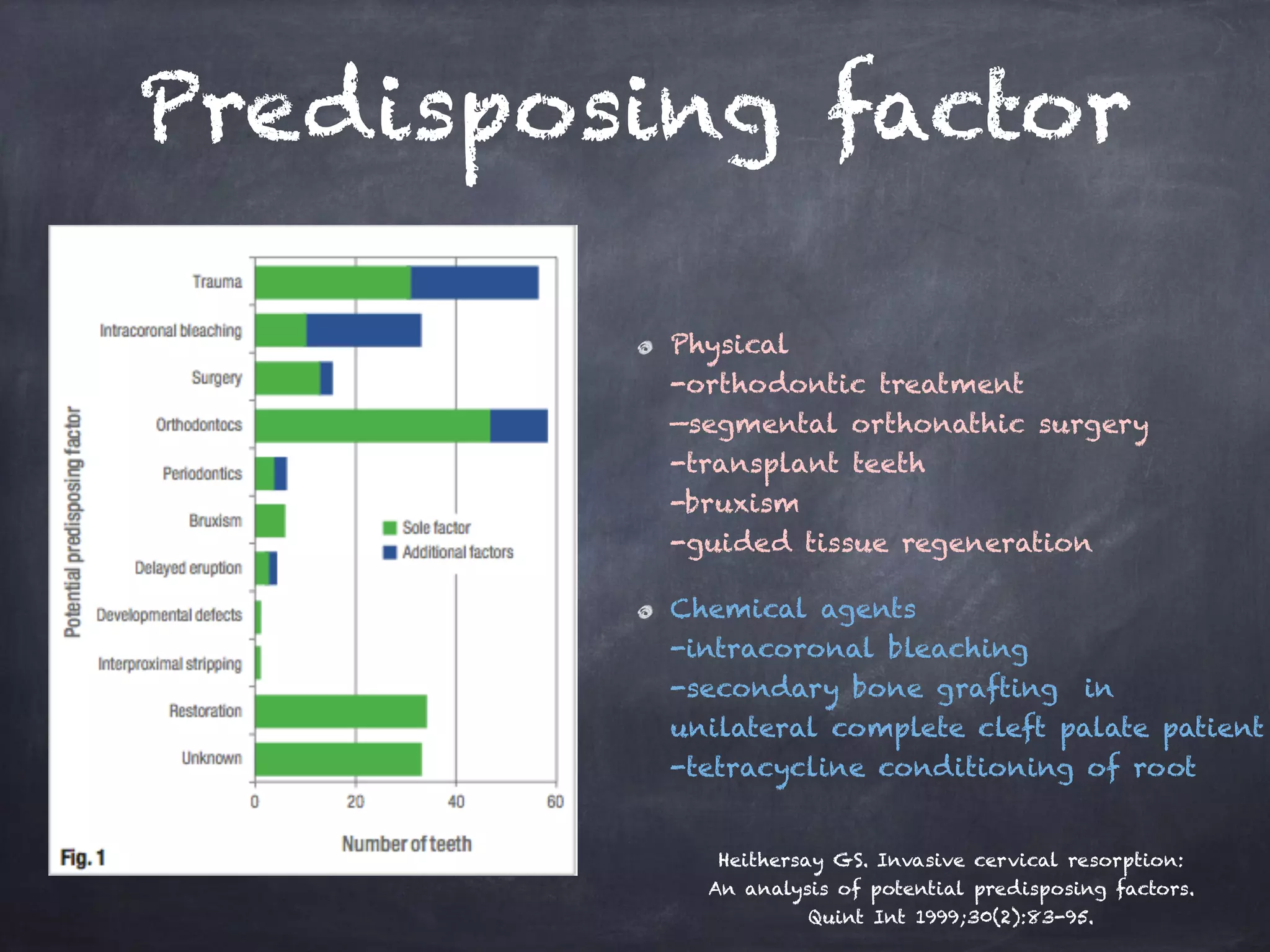
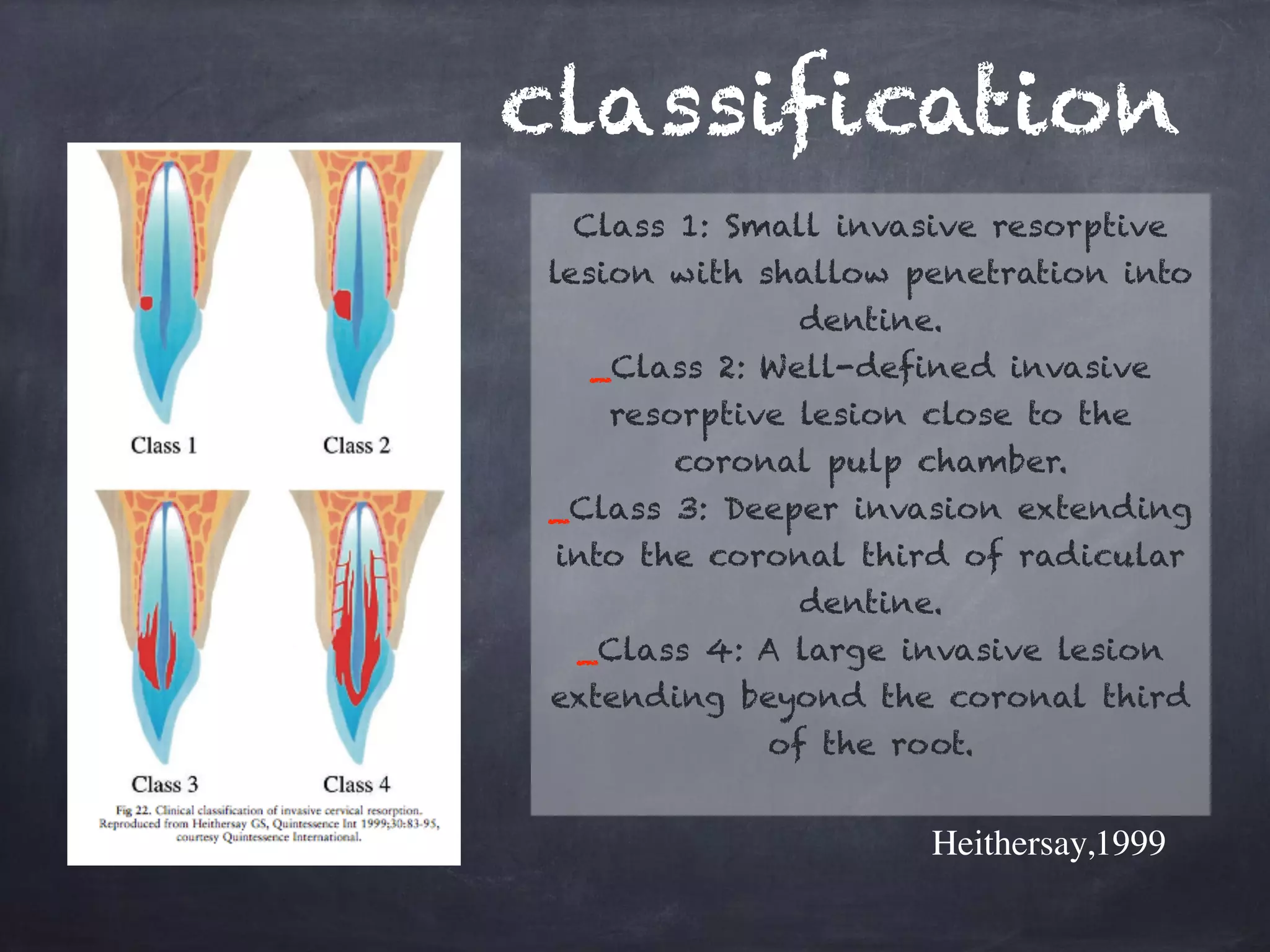
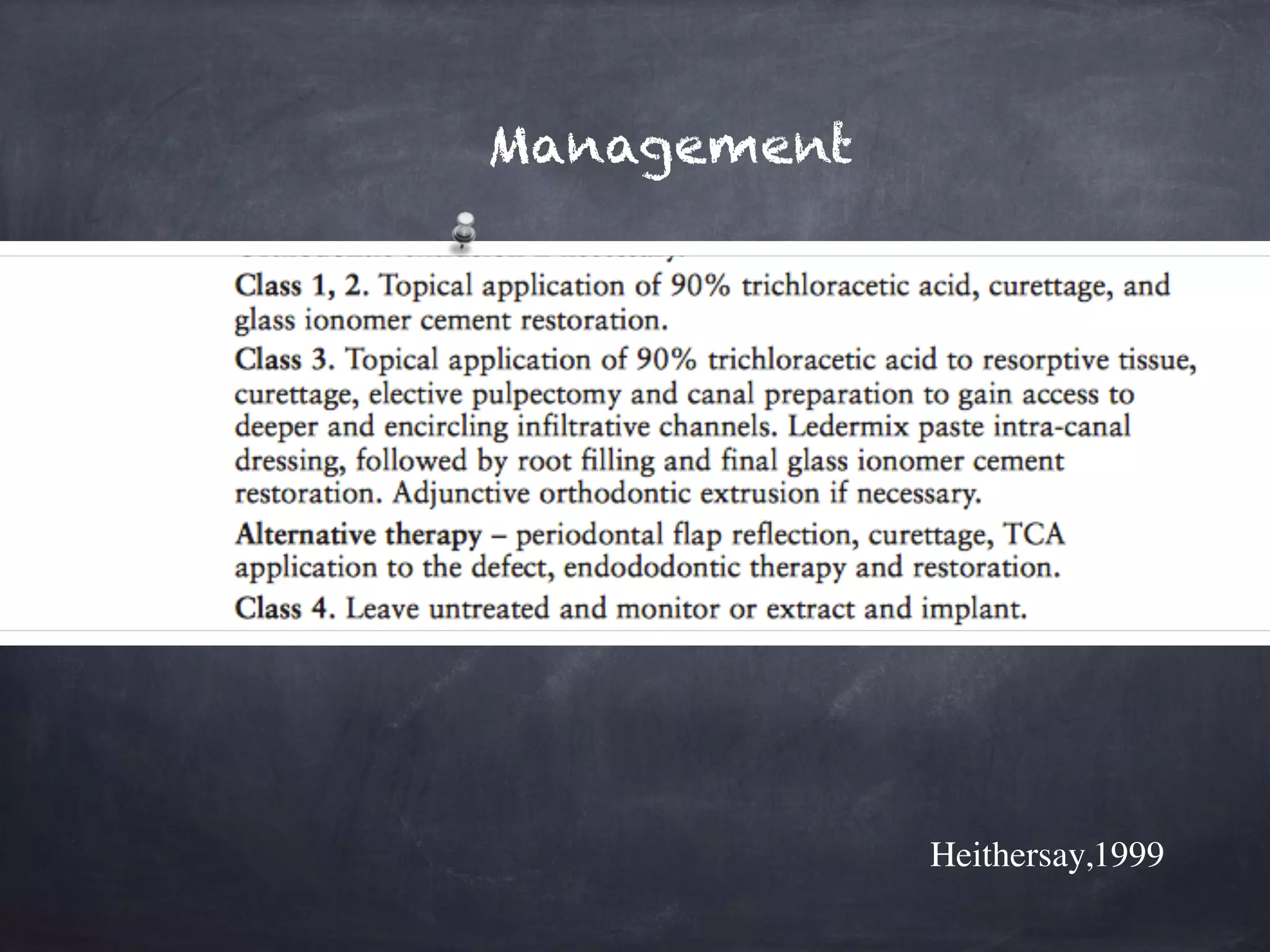
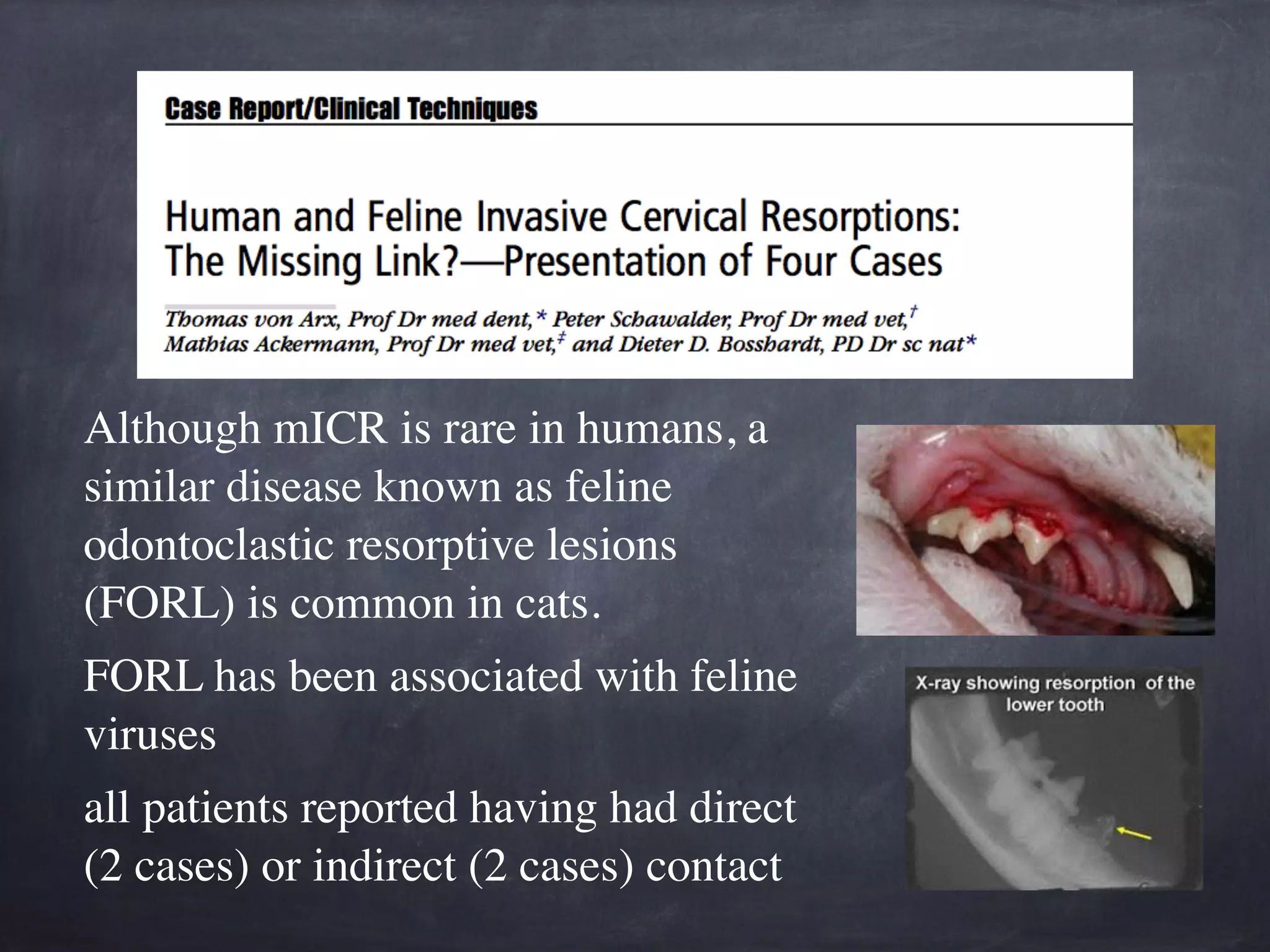
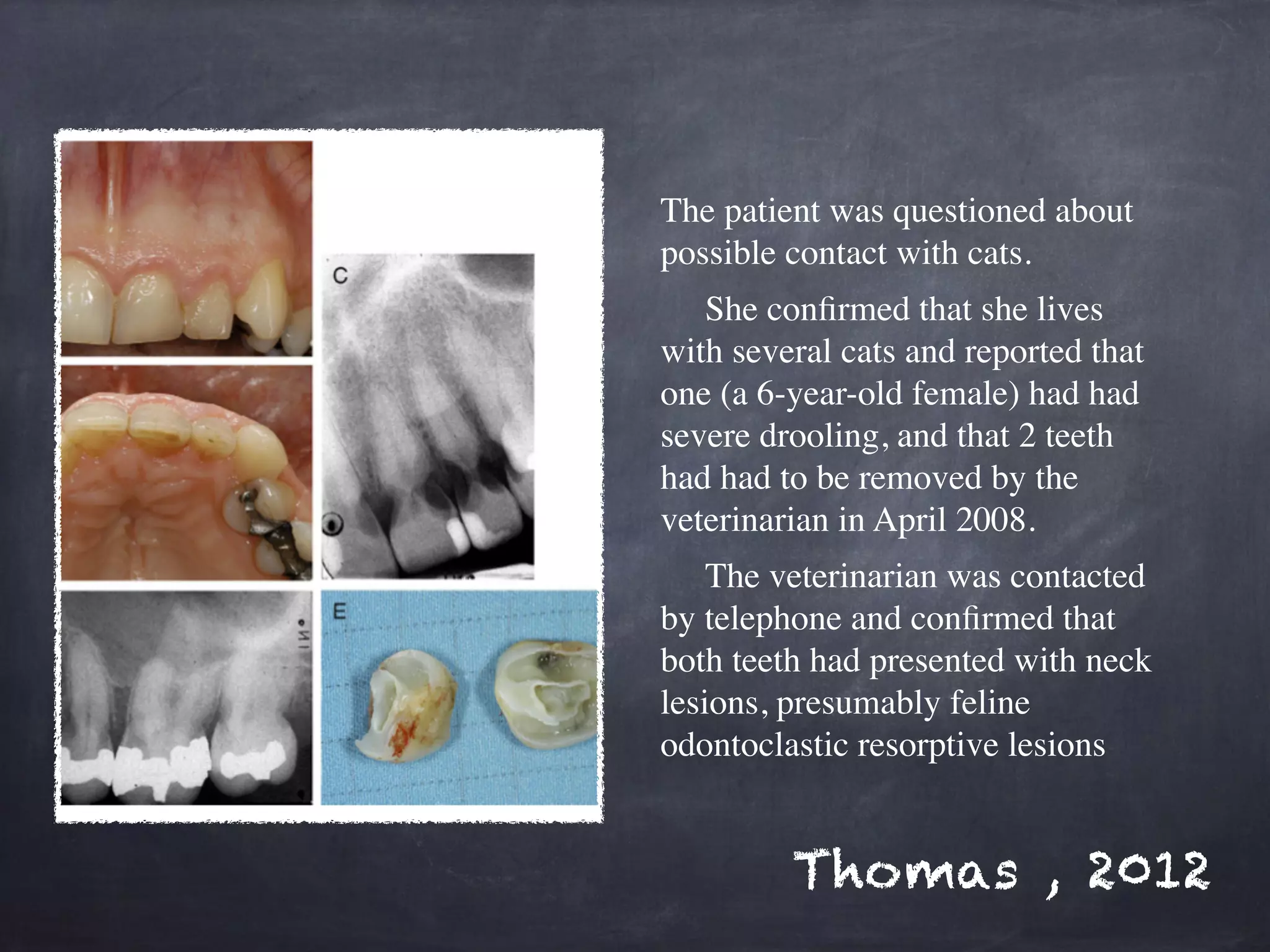
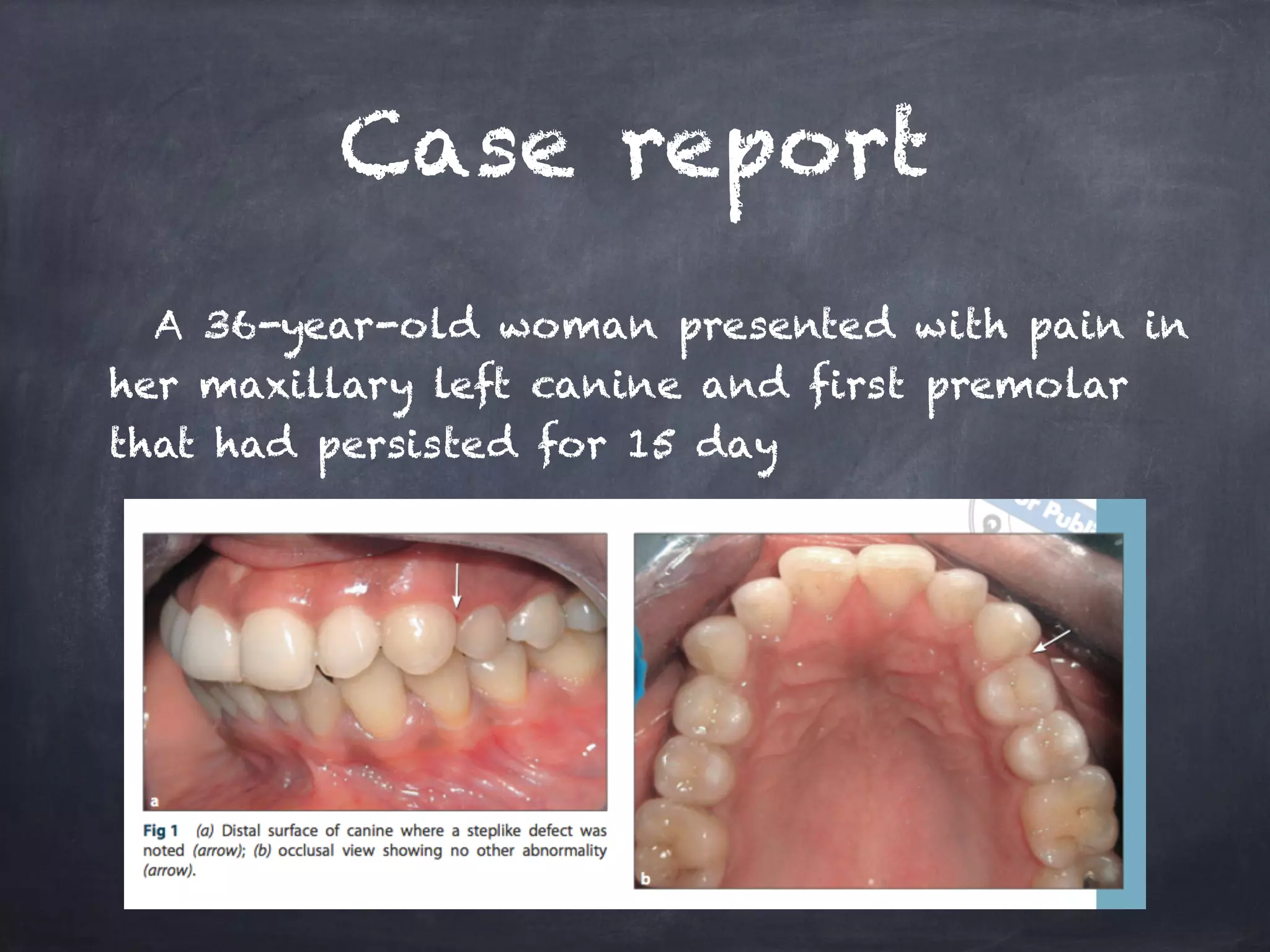
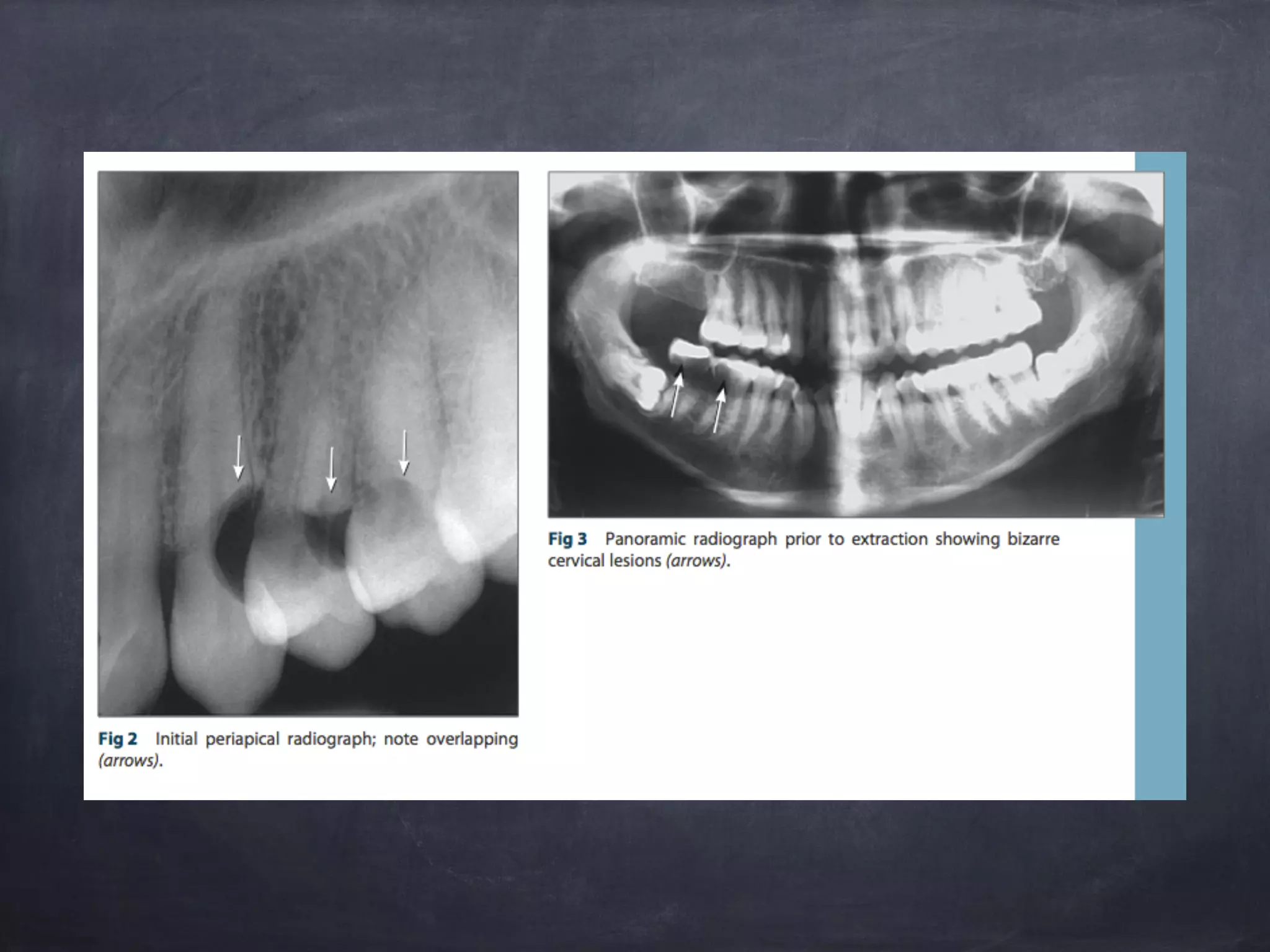
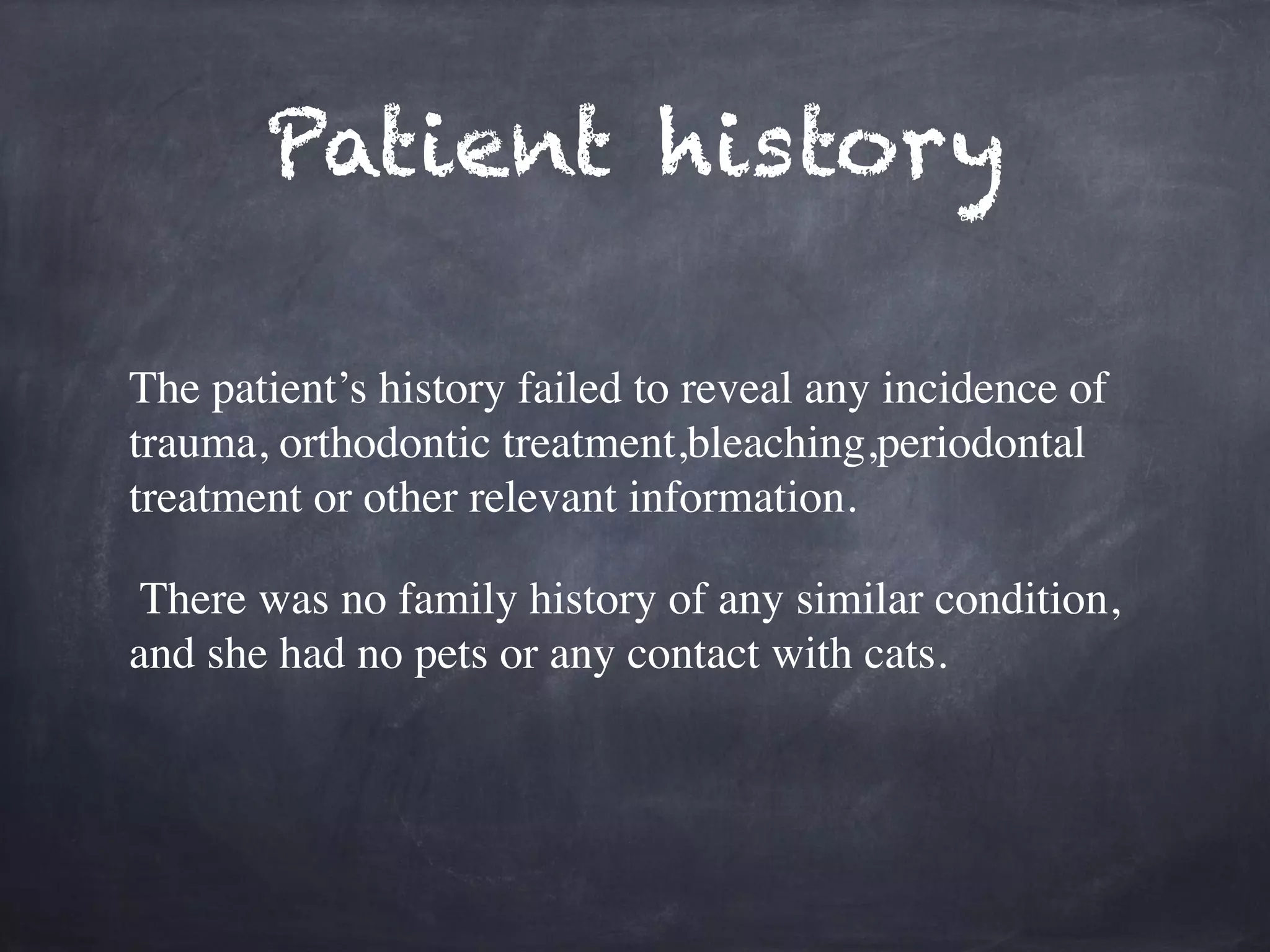
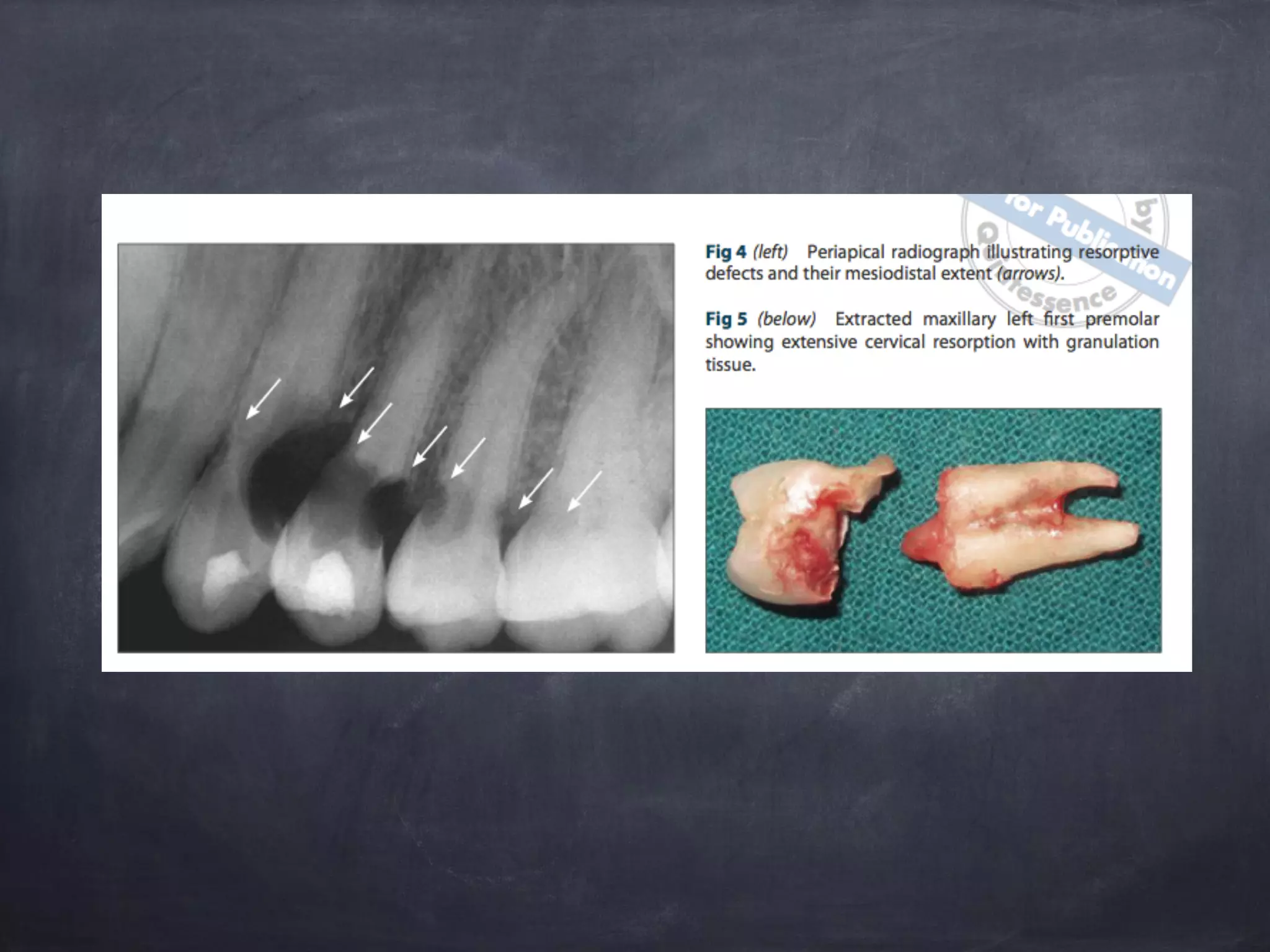
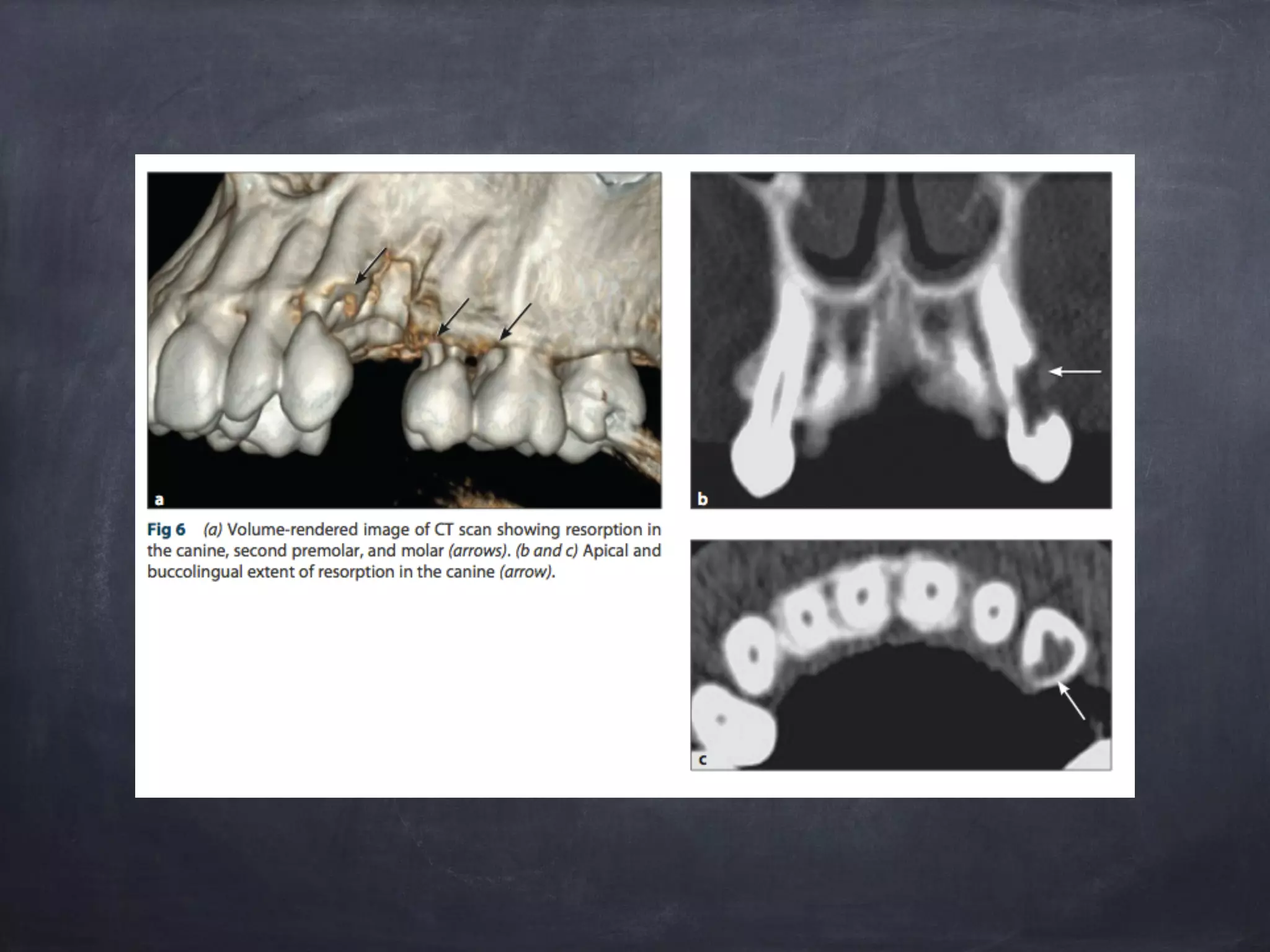
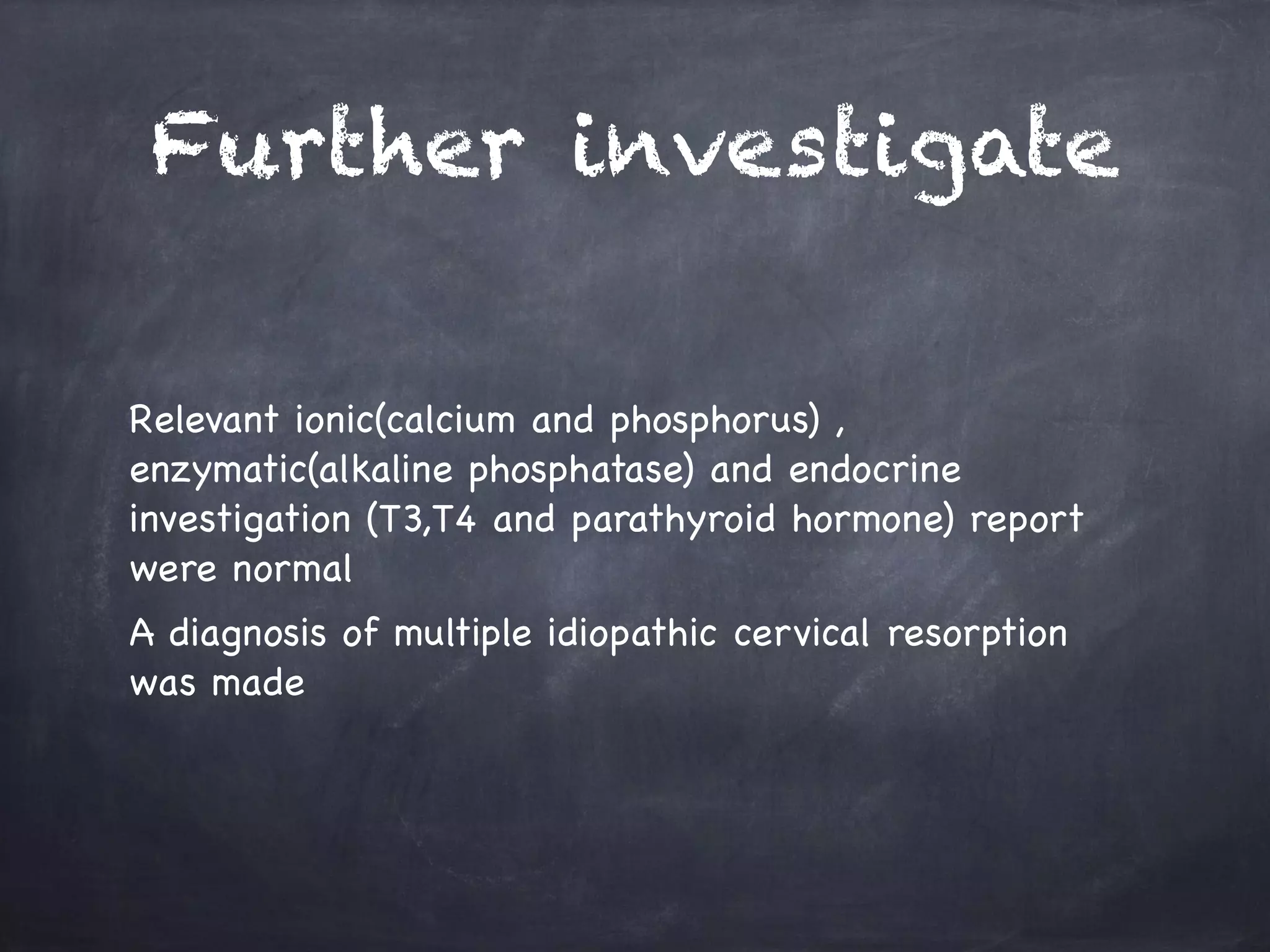
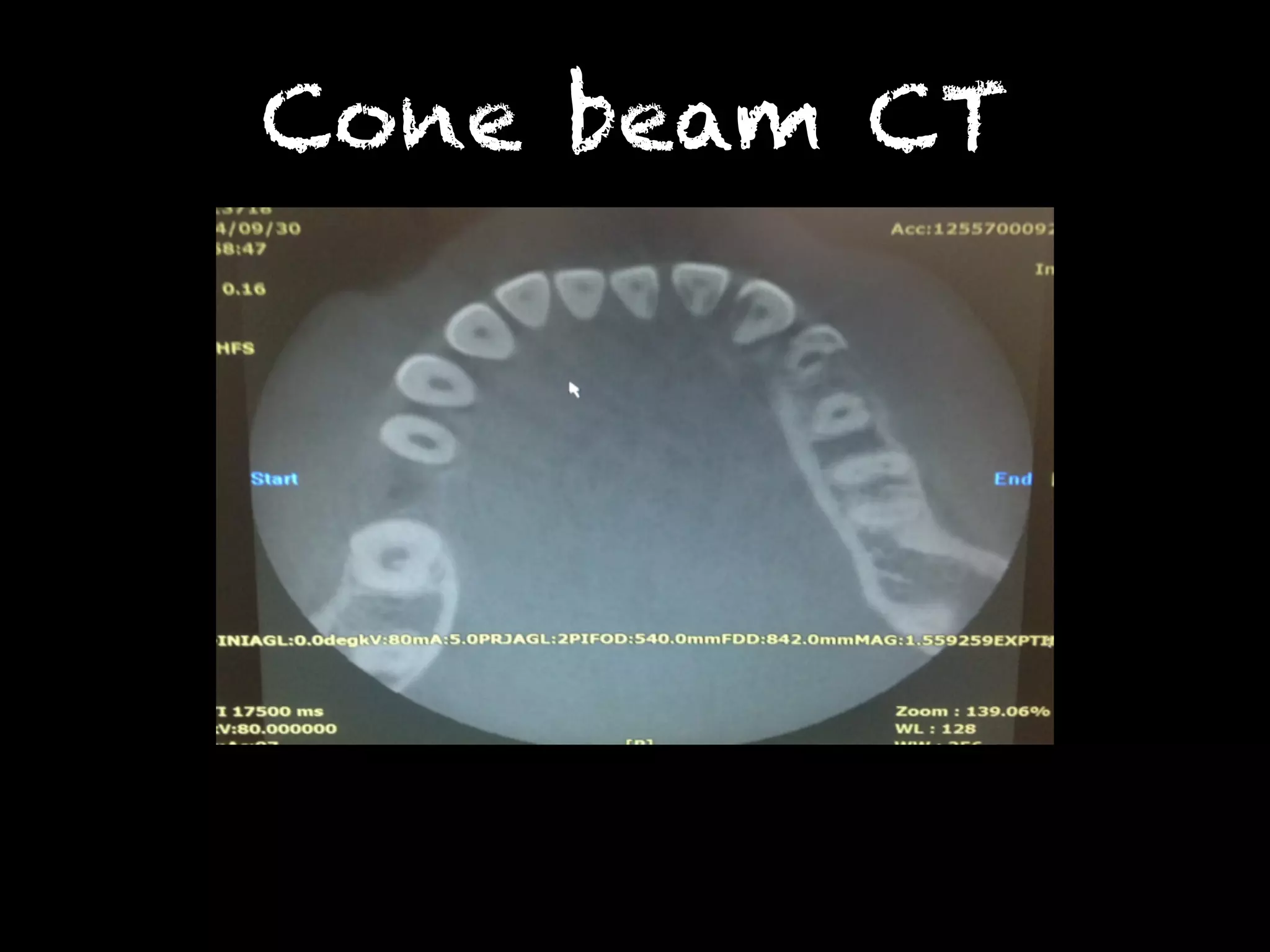
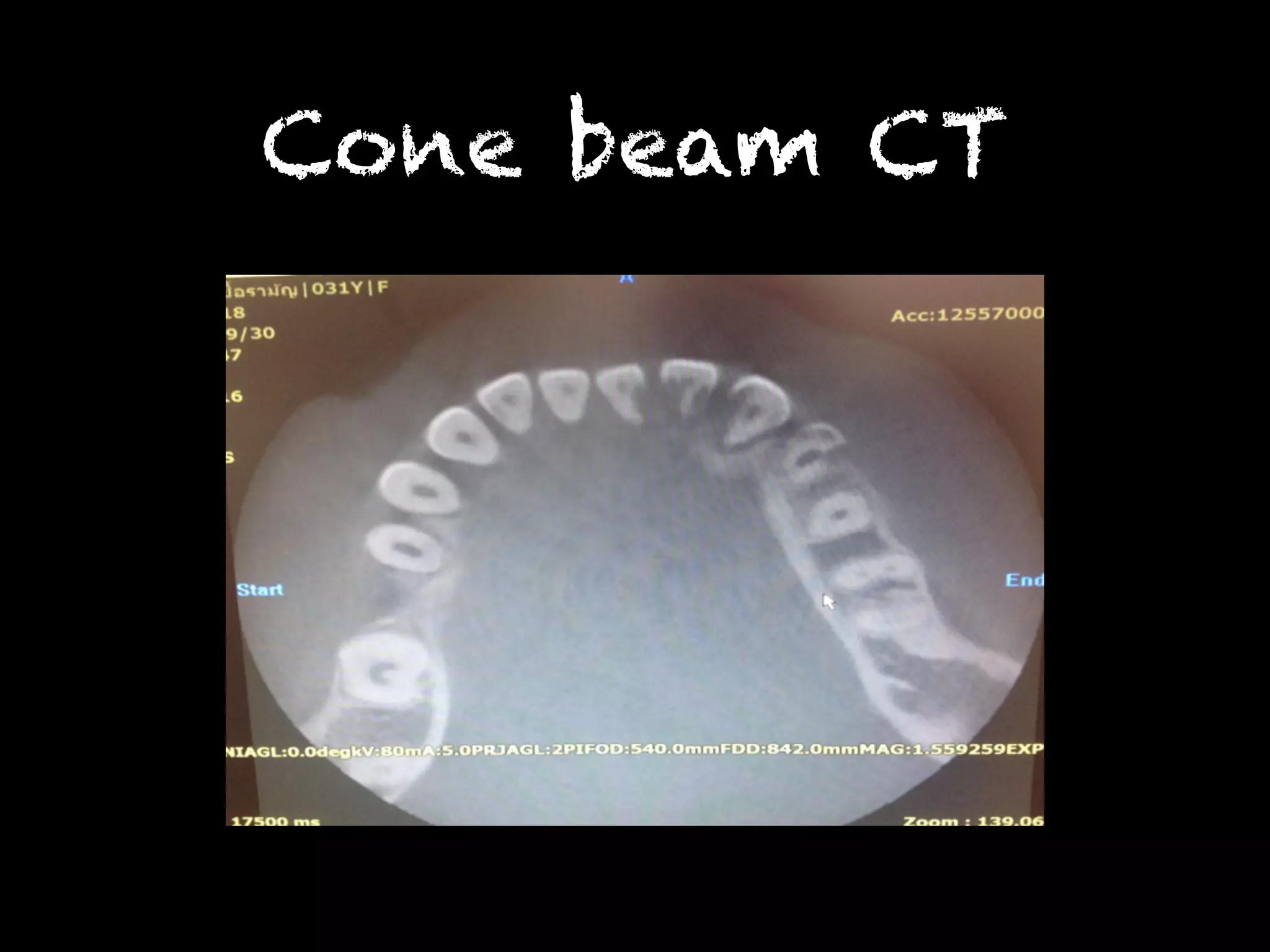
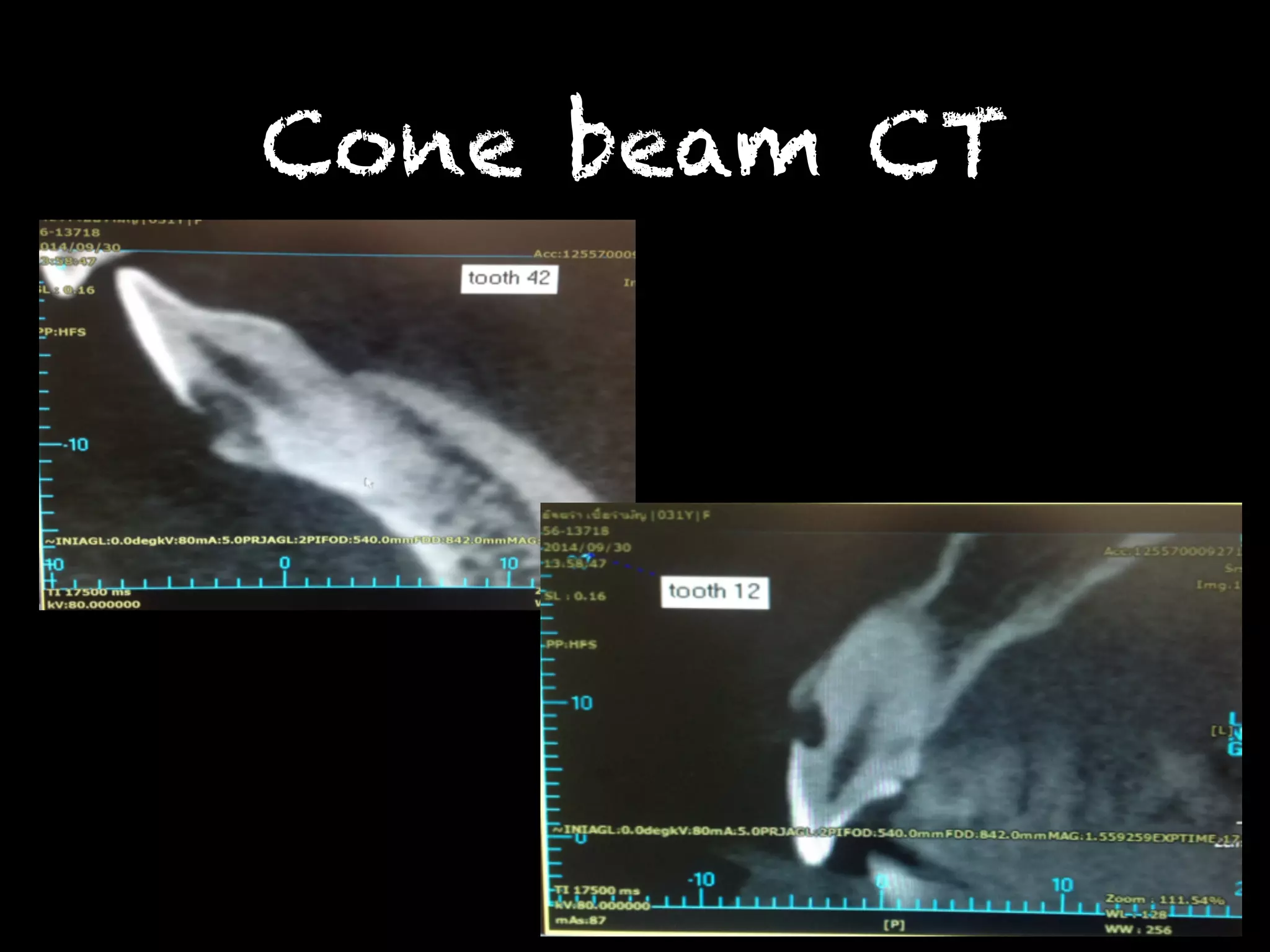
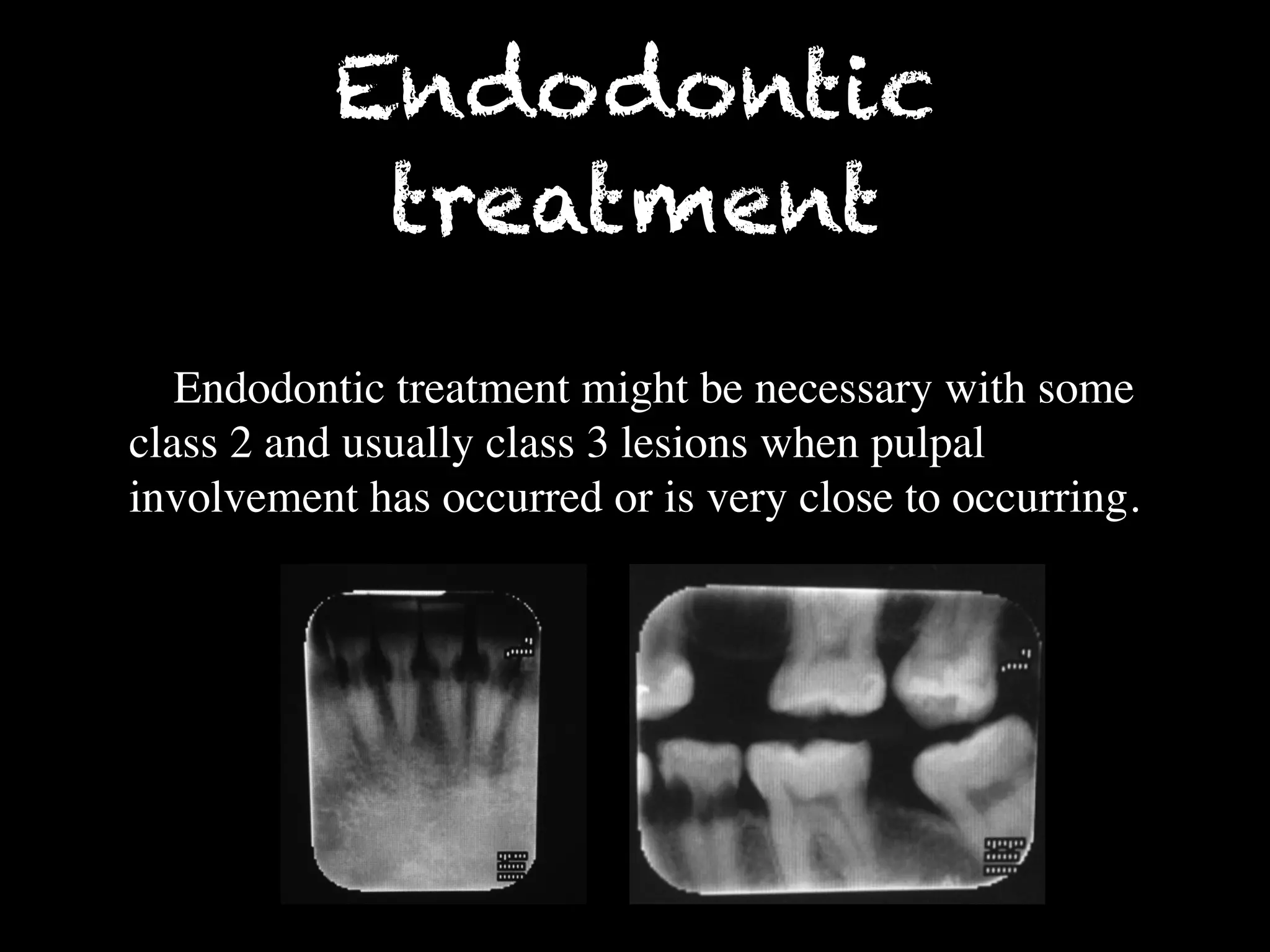
This document summarizes a dental case conference regarding a 31-year-old female patient presenting with multiple invasive cervical resorptions. Examination found lesions on several teeth. The differential diagnosis included dental caries and root resorption. Further radiographic examination and consultation with a radiologist supported a diagnosis of multiple invasive cervical resorption. This type of resorption is rare in humans but similar to a condition seen in cats caused by feline viruses. The patient confirmed contact with cats, one of which had recent dental issues, supporting possible transmission of a virus. Treatment options for this condition were discussed.