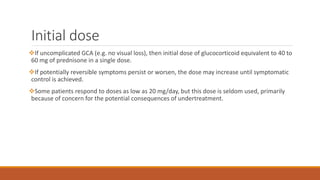
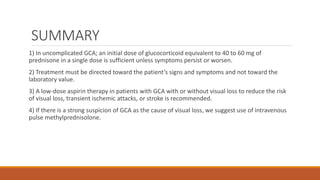
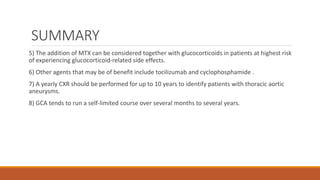
1) Treatment for giant cell arteritis involves promptly starting glucocorticoids such as prednisone once diagnosed, even if biopsy results are pending, to prevent vascular complications.
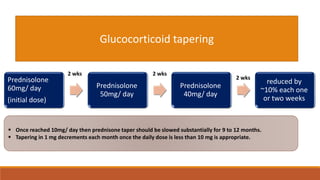
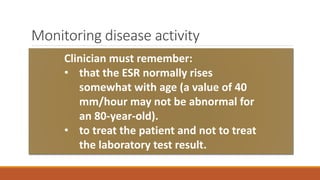
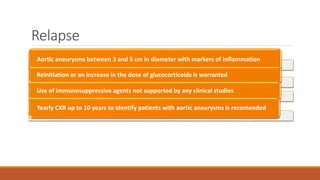
2) Monitoring of inflammatory markers and symptoms is important when tapering glucocorticoid doses to watch for relapse.
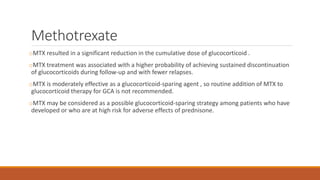
3) Methotrexate or other immunosuppressants may help reduce glucocorticoid doses for patients at high risk of side effects or with resistant disease.