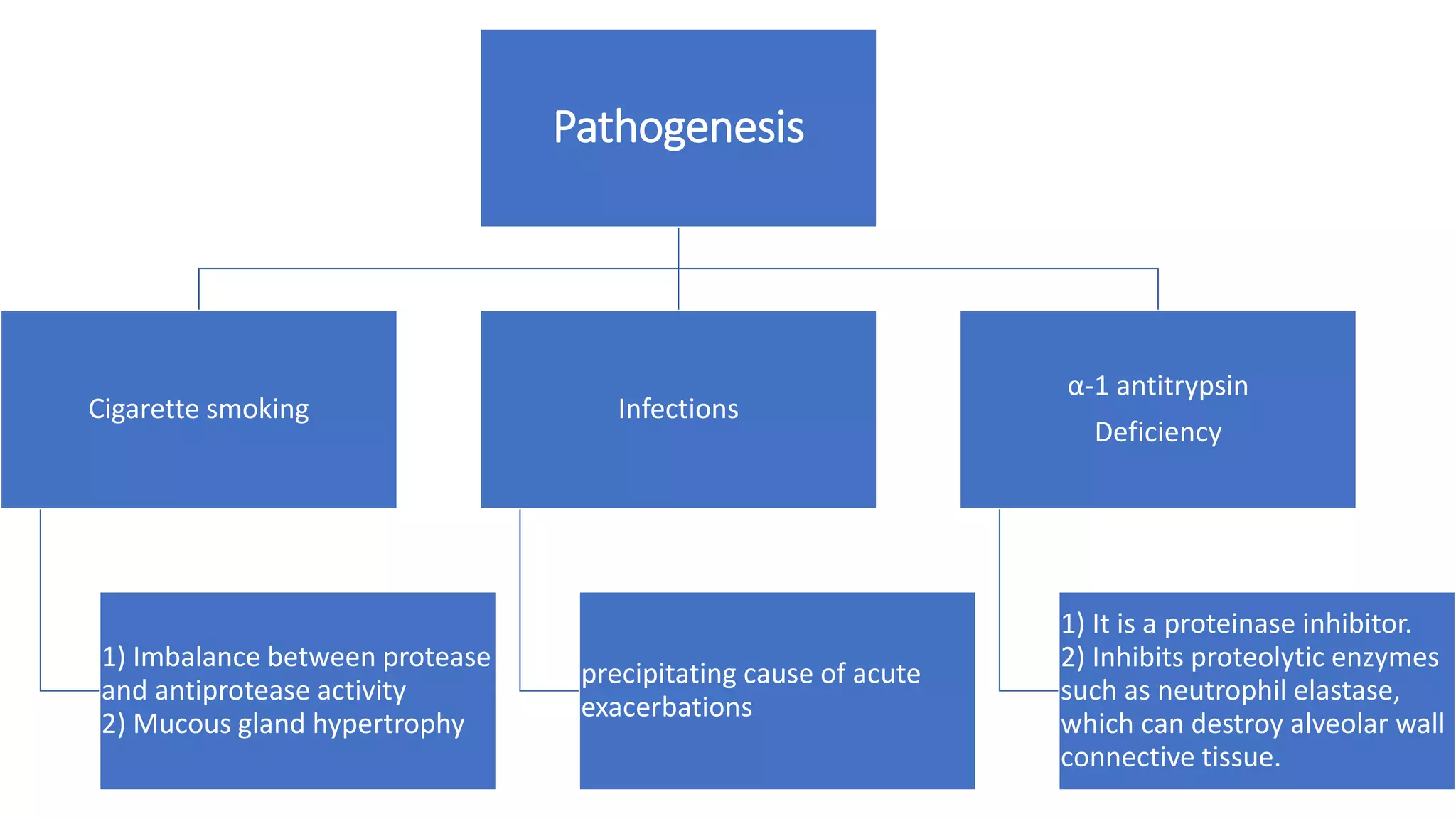
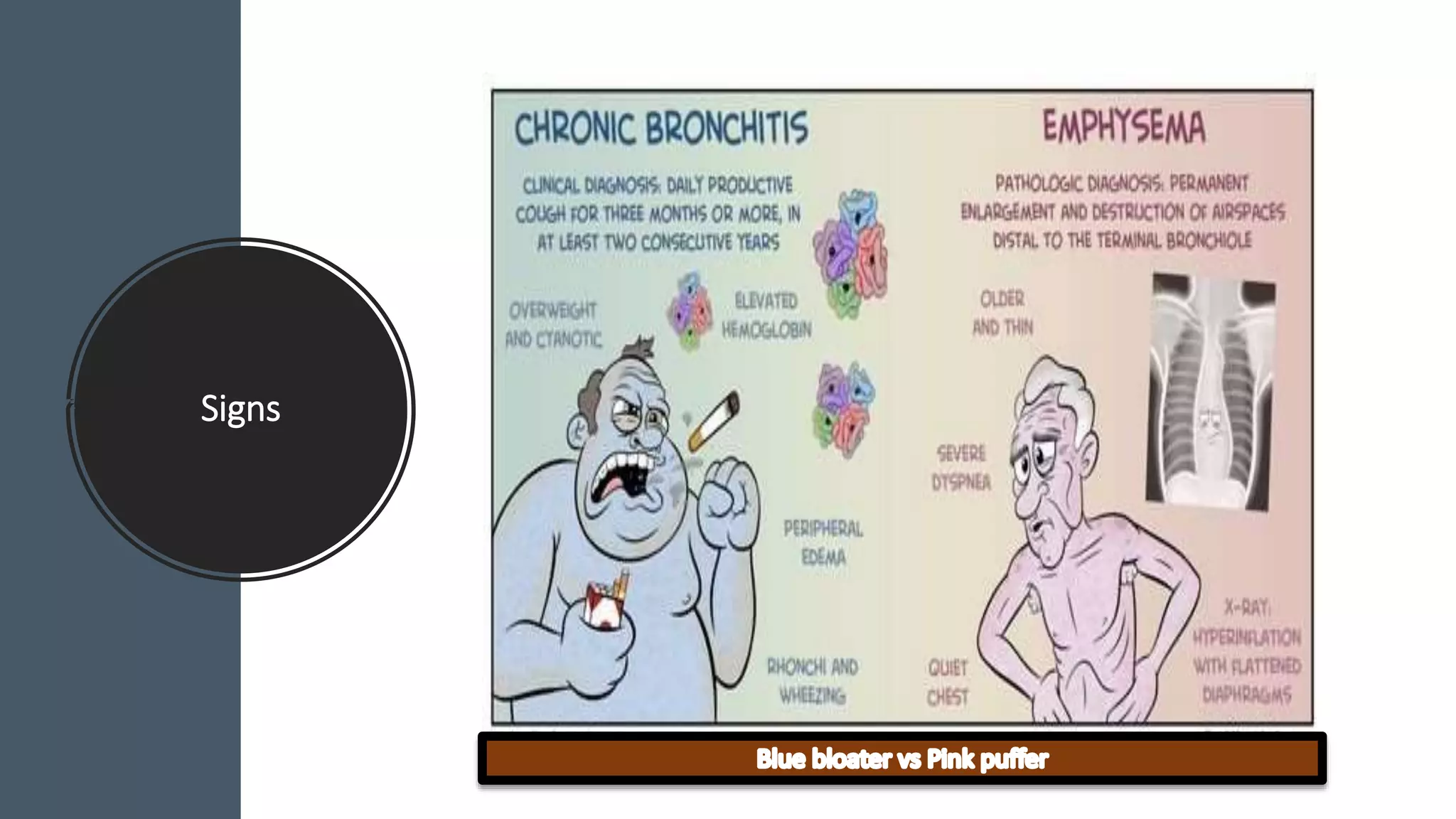
Chronic Obstructive Pulmonary Disease (COPD) is an irreversible lung disease characterized by limited airflow and an abnormal inflammatory response in the lungs caused by long-term exposure to harmful particles like cigarette smoke. The main symptoms are breathlessness, cough, and wheezing. Diagnosis is based on a history of symptoms and cigarette smoking, and confirmed with lung function tests showing reduced airflow. Treatment focuses on smoking cessation and drug therapy with bronchodilators and corticosteroids to manage symptoms and reduce exacerbations.