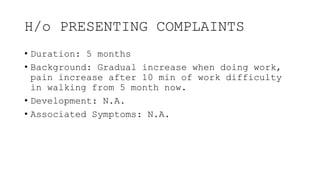
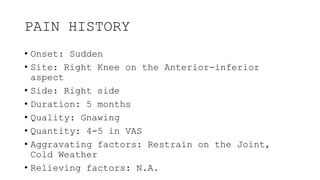
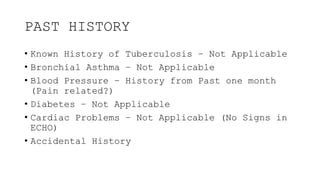
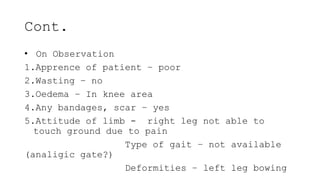
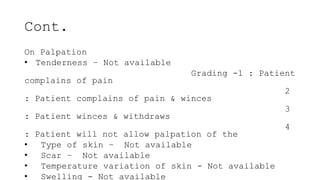
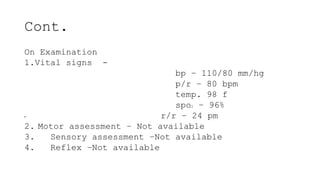
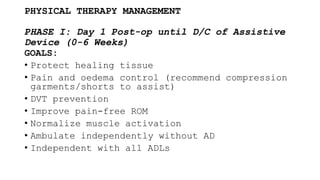
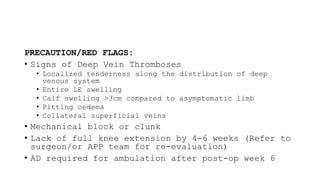
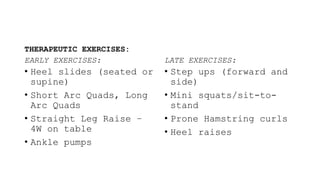
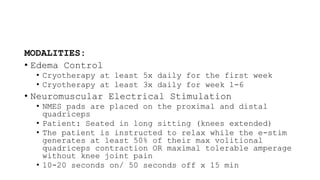
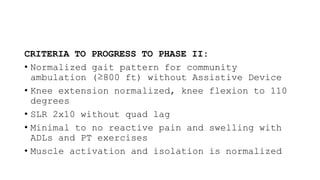
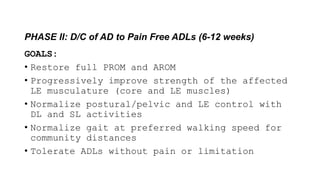
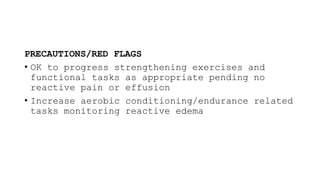
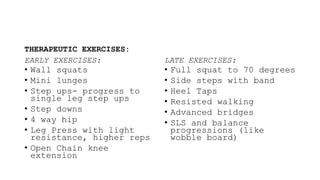
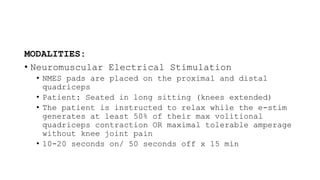
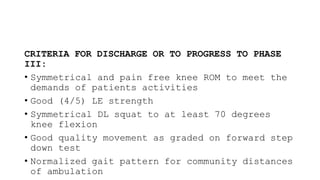
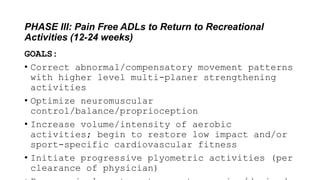
The document presents a case study of a 75-year-old male patient experiencing difficulty walking and pain in the right knee for five months, with a history of associated symptoms and no significant past medical history. It outlines the physical examination, findings, and a detailed physical therapy management plan divided into phases focused on rehabilitation goals, therapeutic exercises, and precautions to ensure patient recovery. Key assessments aim to restore functionality and strengthen the affected leg while monitoring for any complications throughout the recovery process.