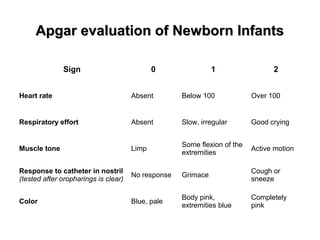
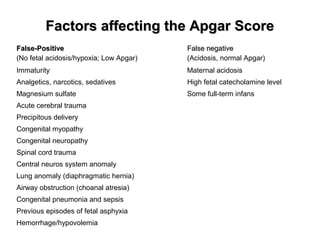
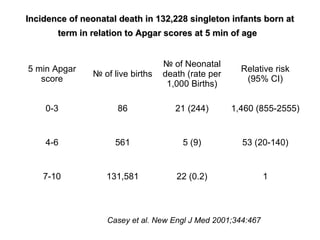
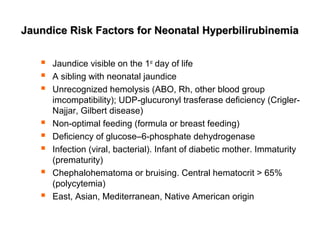
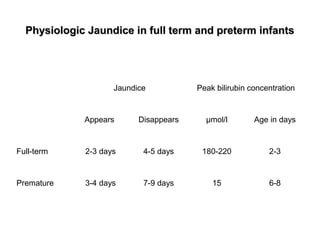
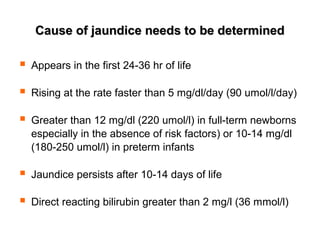
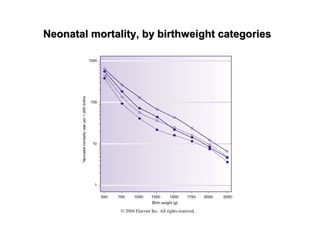
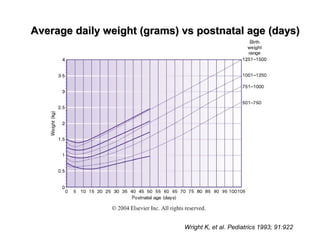
The document discusses Apgar scoring, which evaluates newborns on factors like heart rate, breathing effort, muscle tone, and skin color to assess their transition from fetus to newborn. It notes that various medical factors can affect Apgar scores, either raising or lowering them despite the infant's actual condition. It also presents data showing greatly increased risk of neonatal death for infants with very low 5-minute Apgar scores. Additional sections cover definitions of preterm and postterm birth, risk factors for jaundice, signs that jaundice requires further evaluation, and graphs on neonatal mortality rates and average daily weight gain by postnatal age.