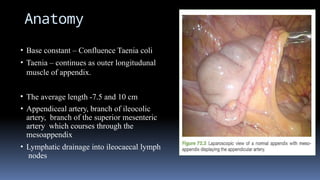
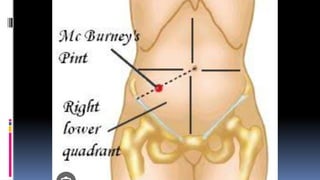
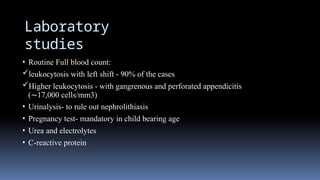
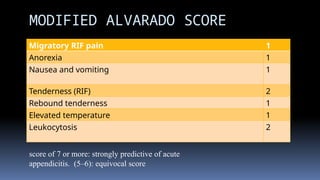
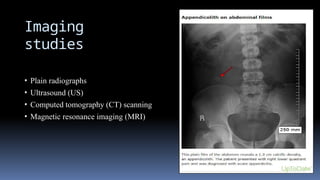
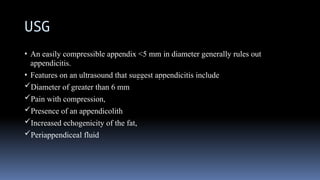
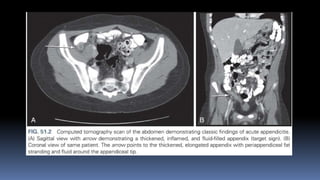
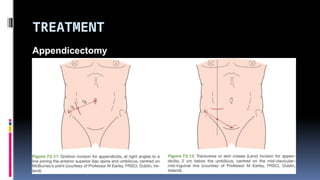
The document provides an overview of acute appendicitis, focusing on its diagnosis, anatomy, and management strategies. It emphasizes the significance of clinical symptoms, laboratory findings, and imaging studies in diagnosing appendicitis, with the modified Alvarado score serving as a predictive tool. Management options include non-operative treatment for uncomplicated cases and multiple surgical approaches for appendectomy.