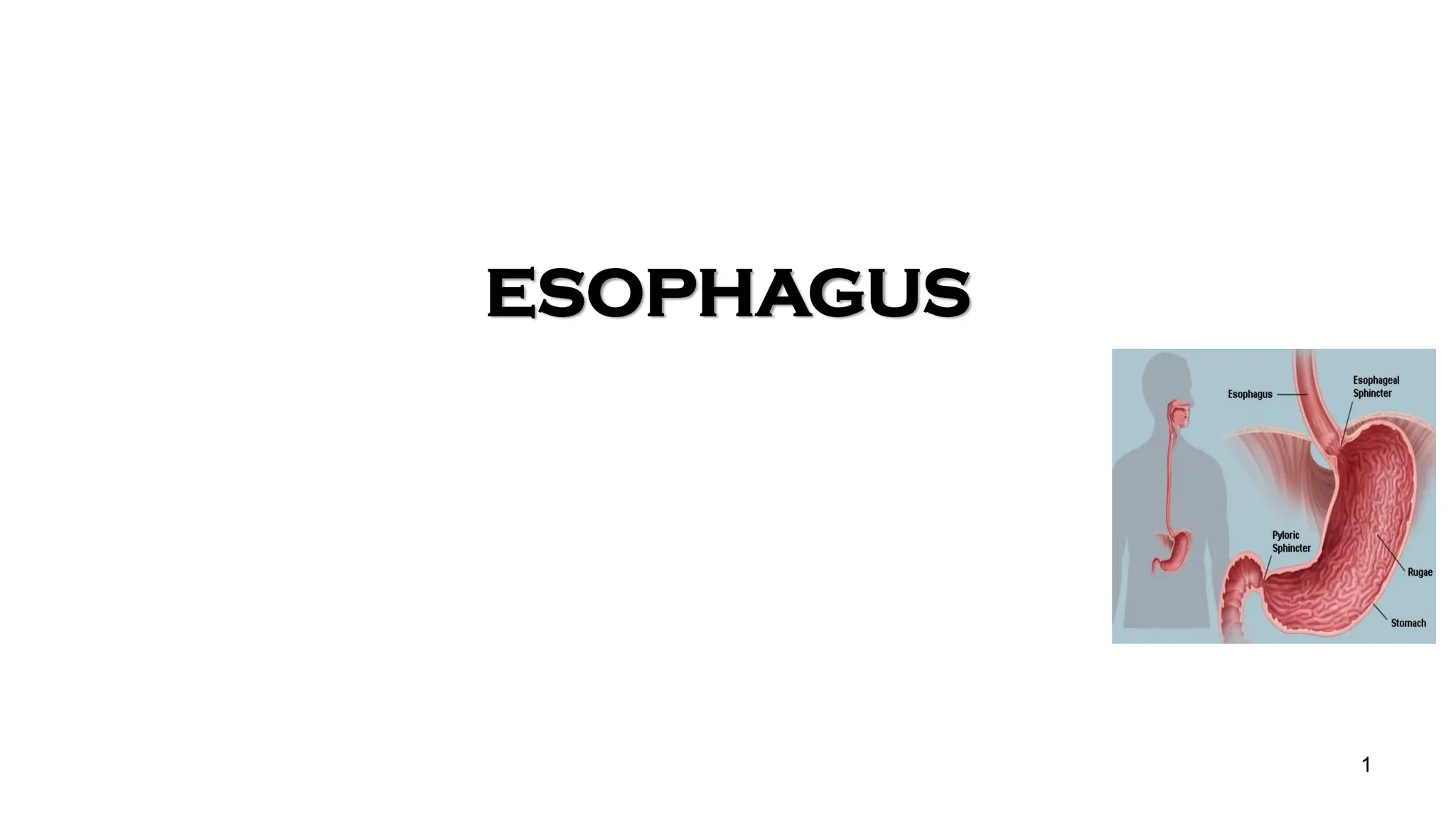
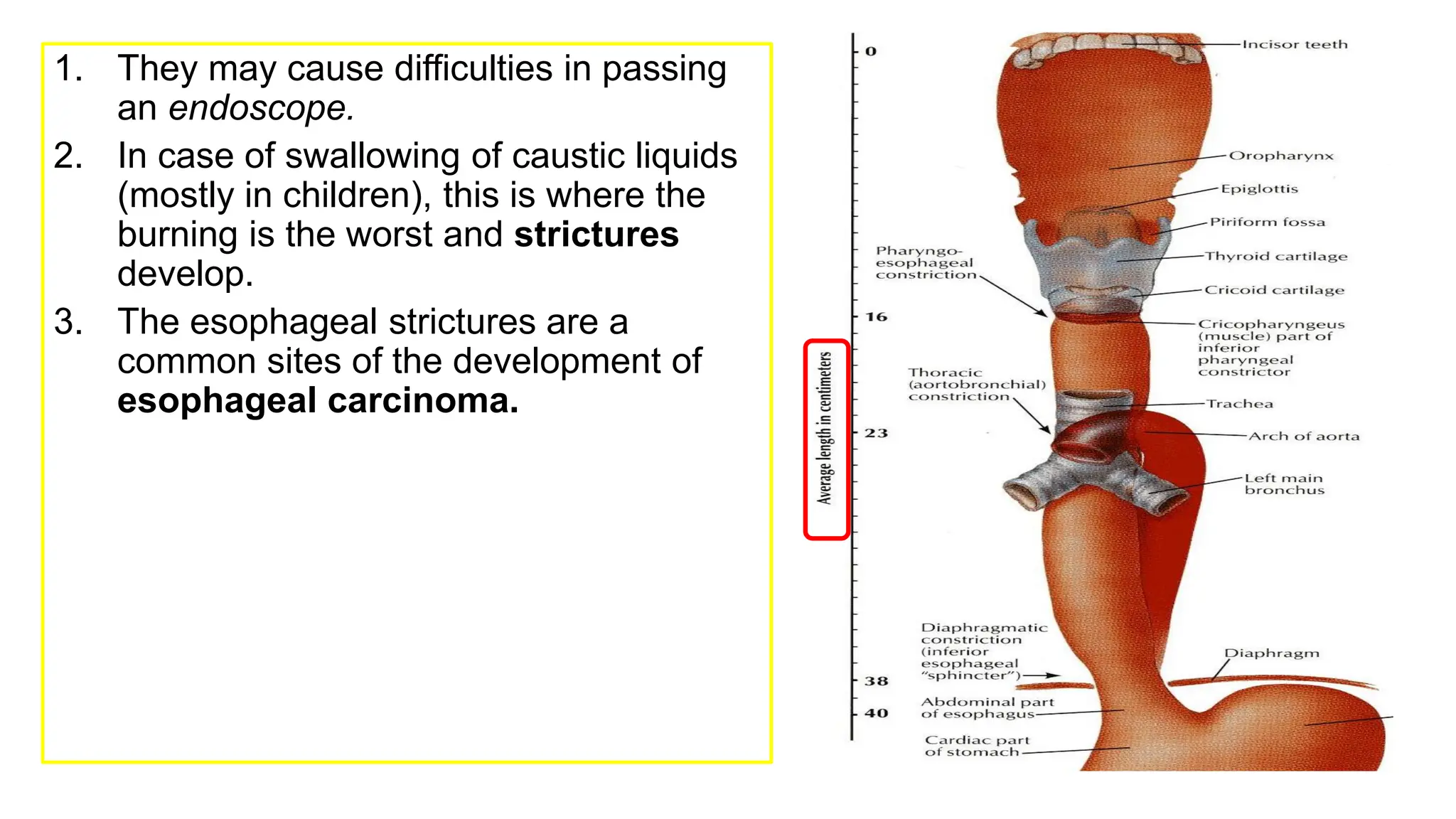
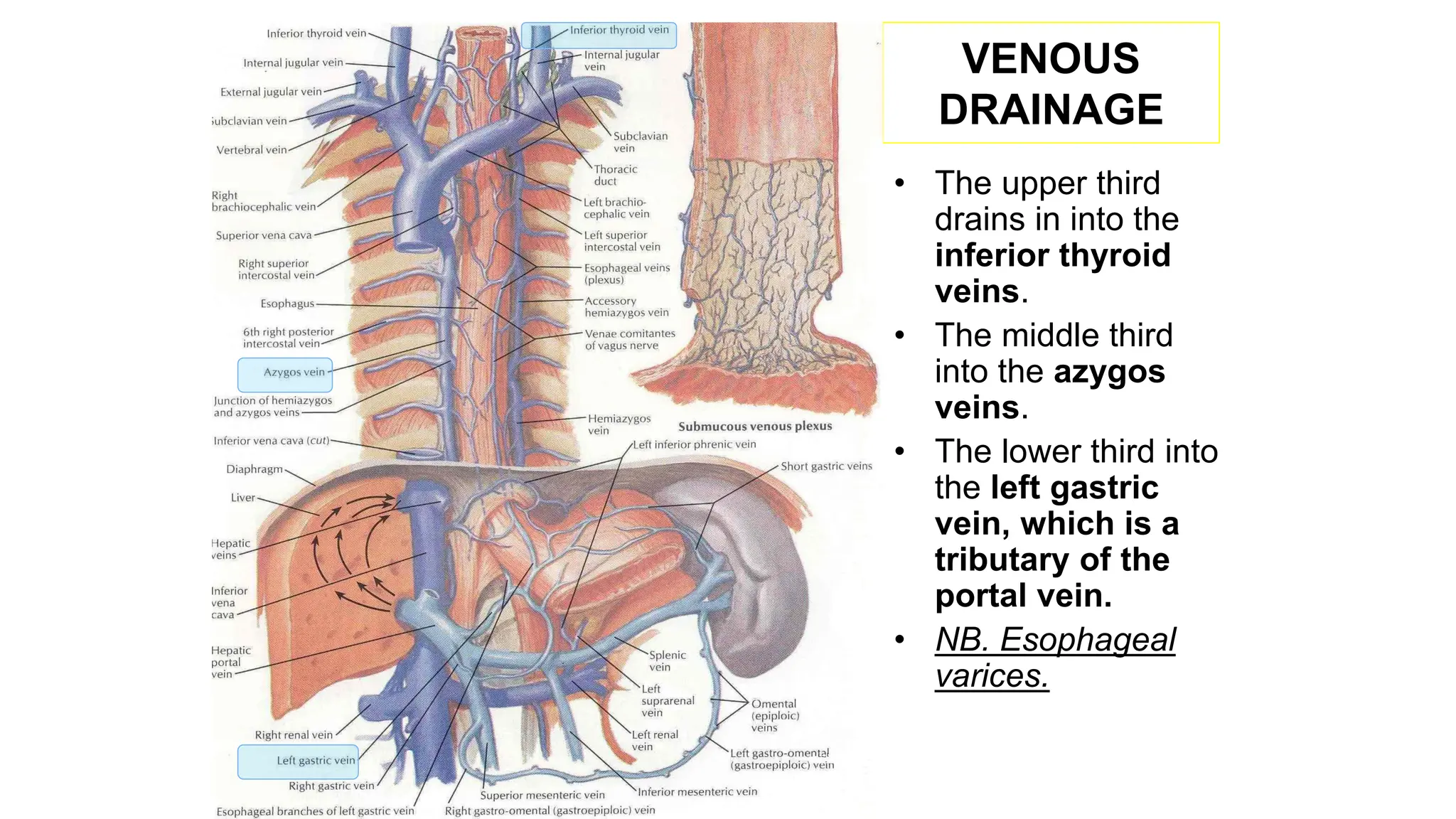
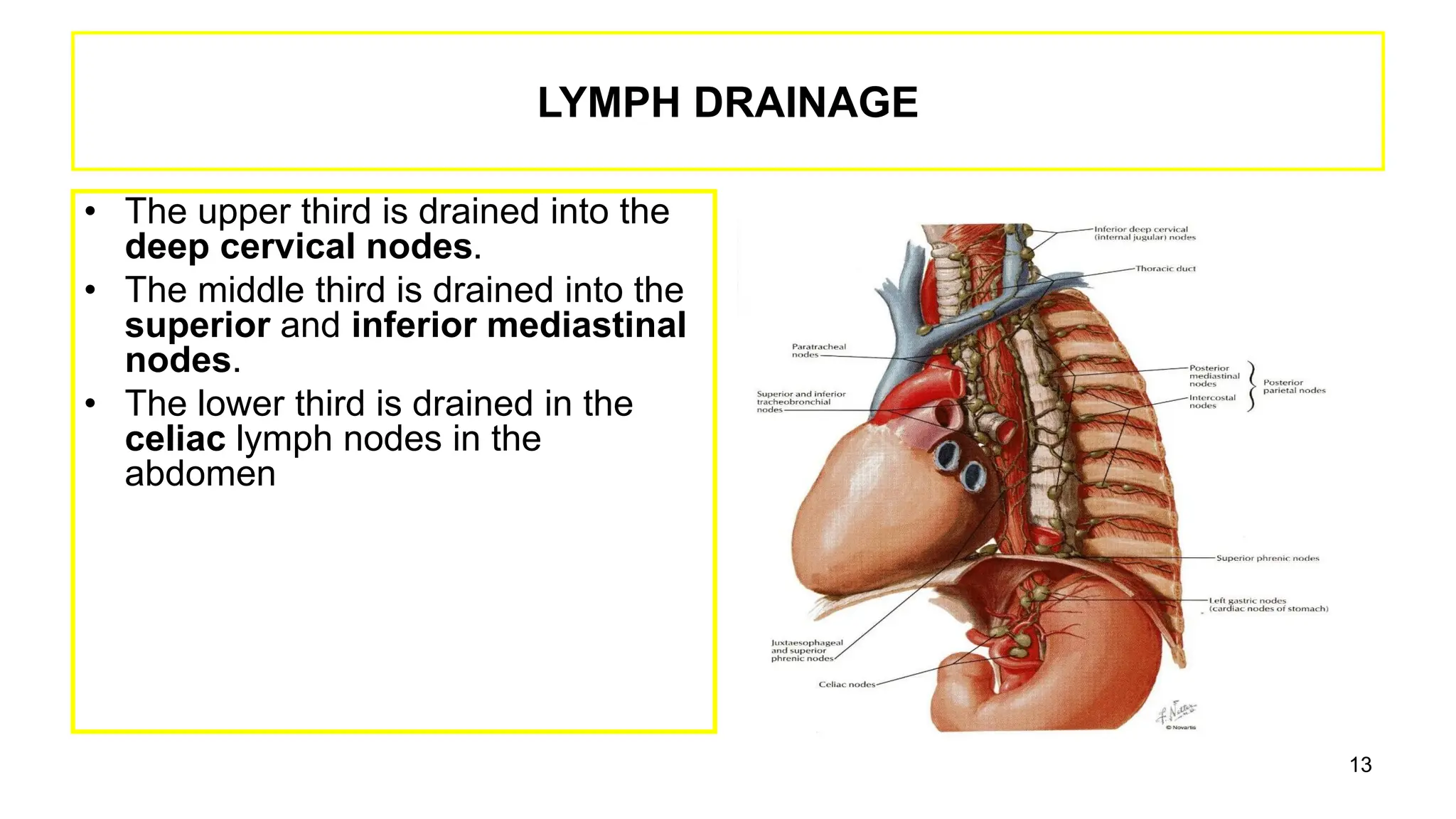
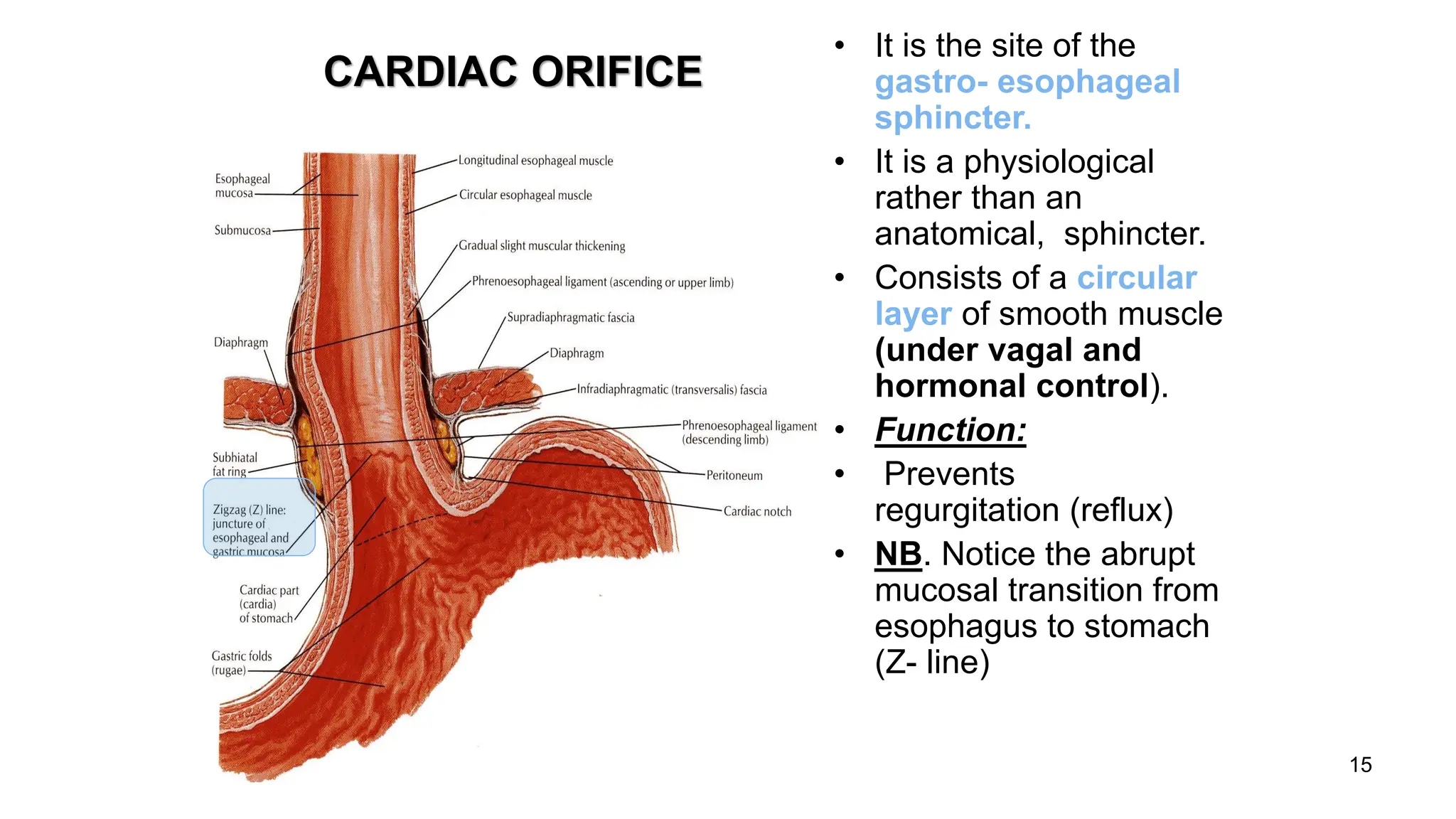
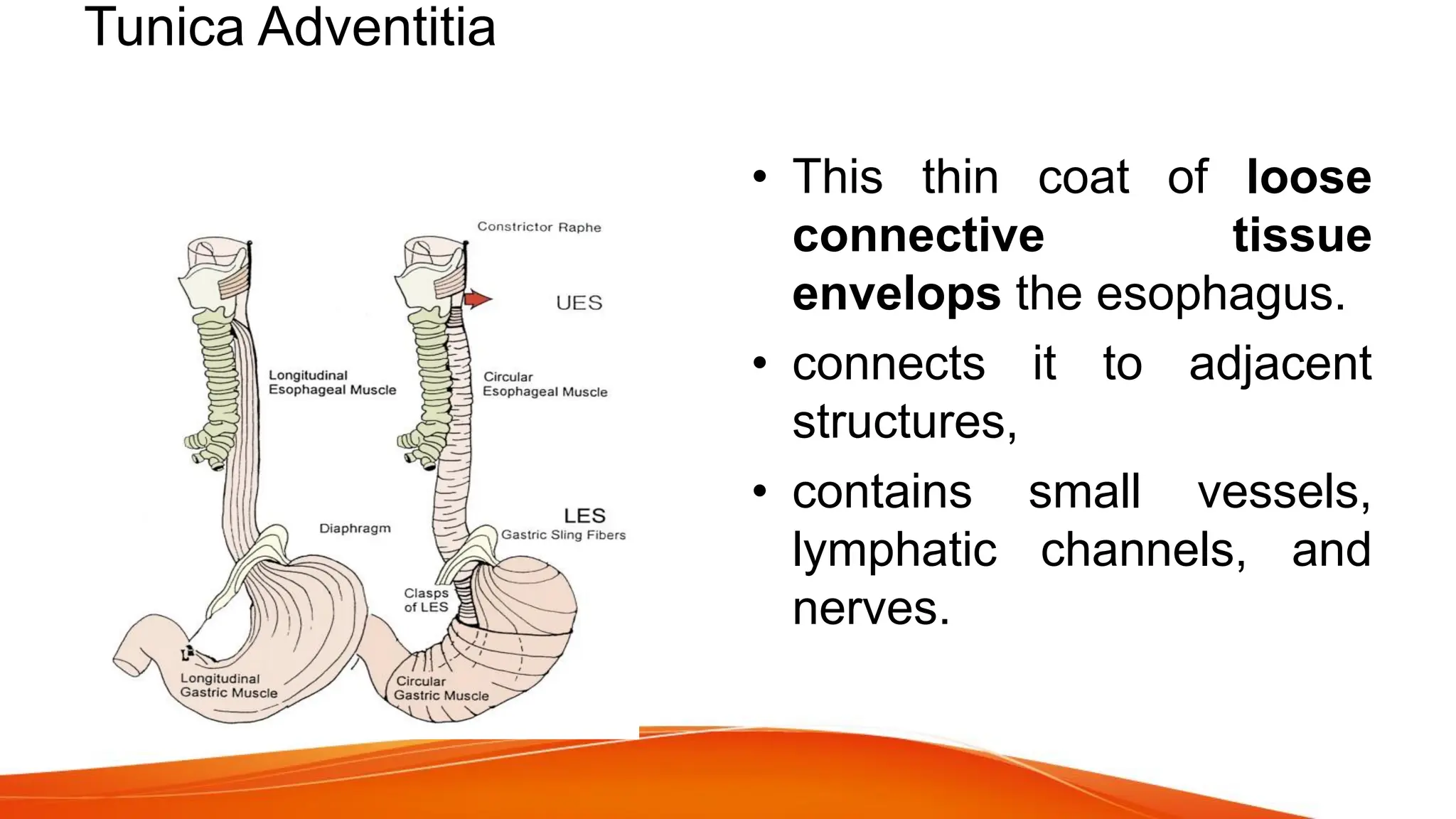
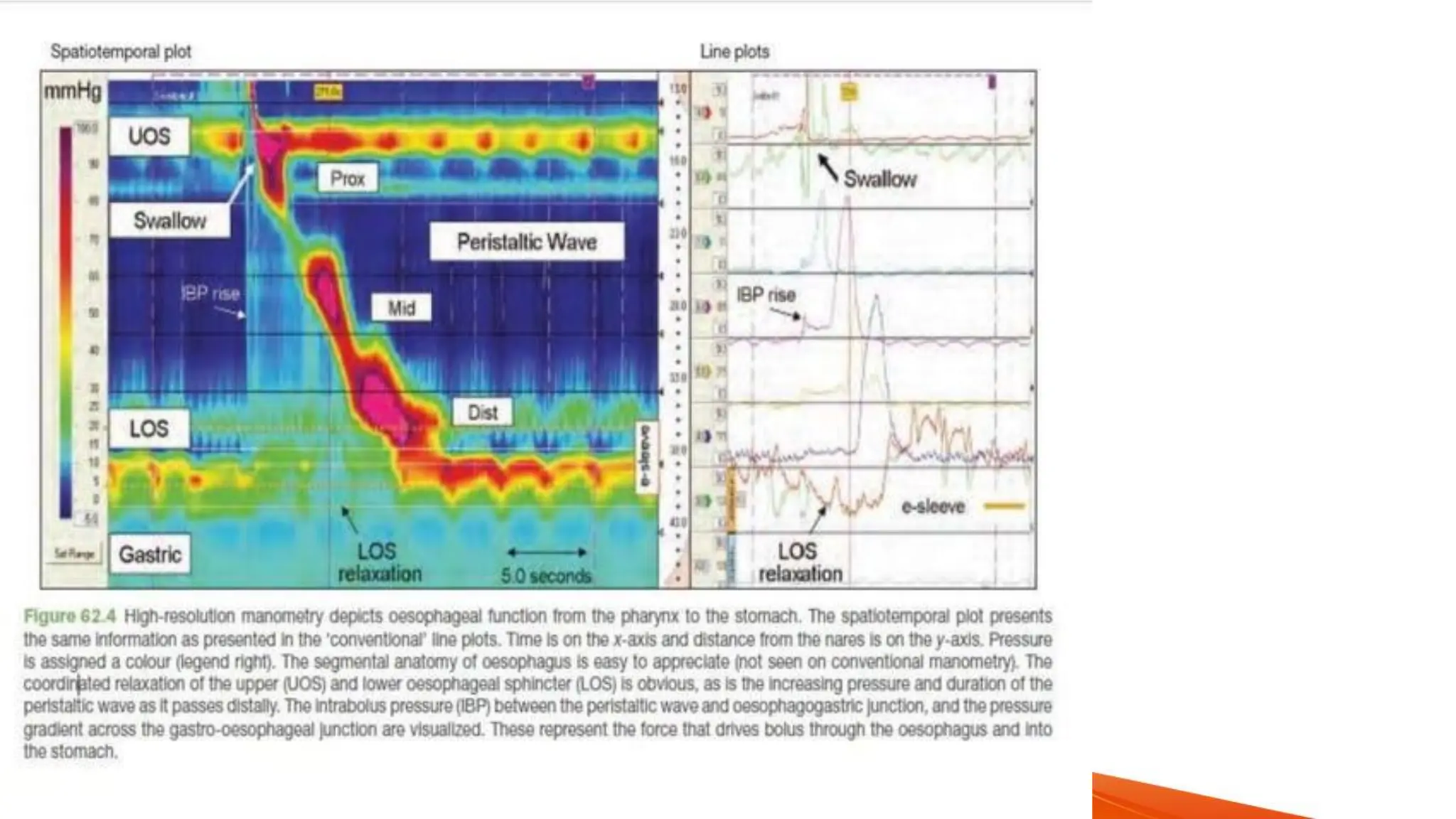
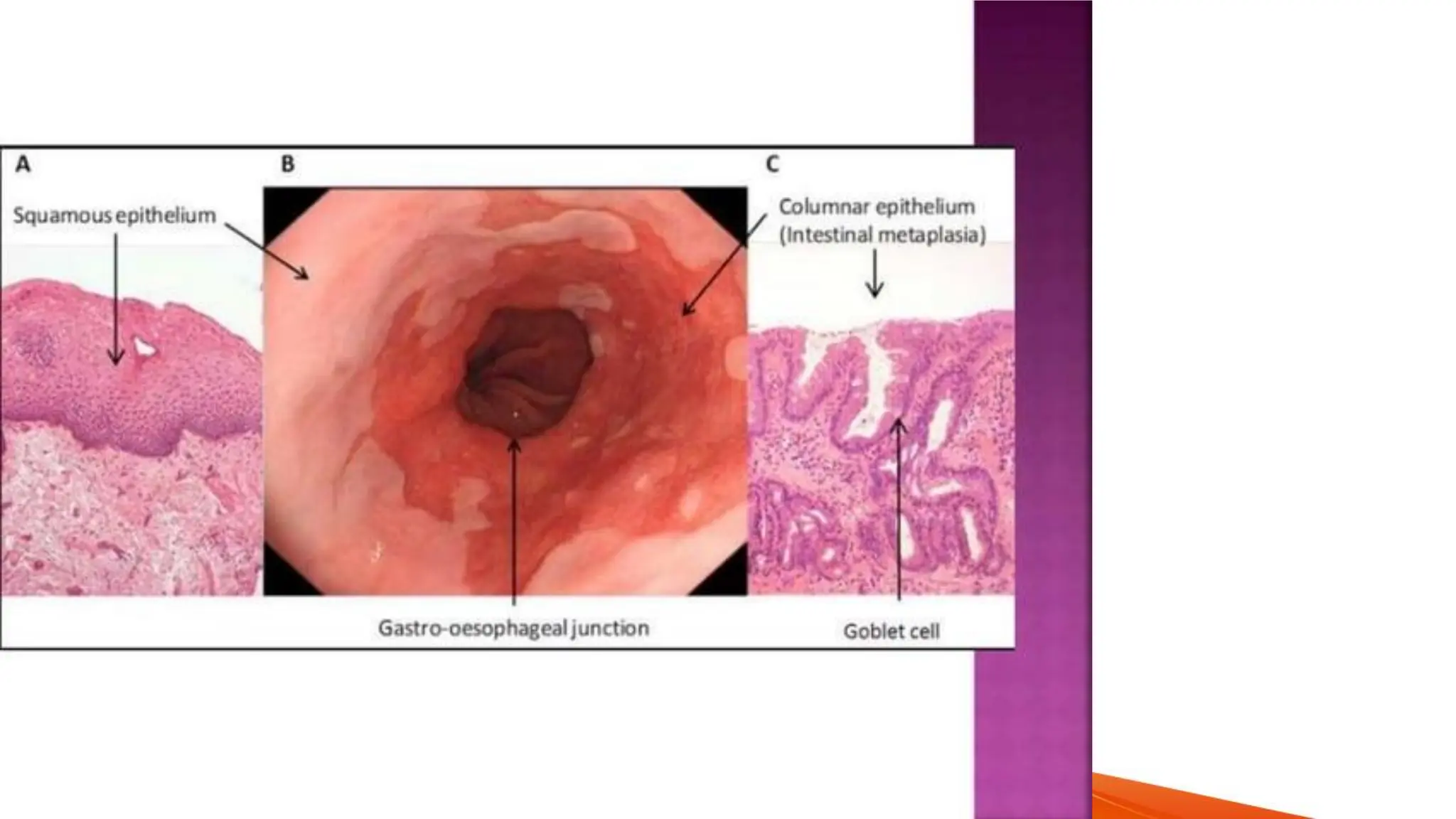
The esophagus, a 25 cm long muscular tube, extends from the pharynx to the stomach and is divided into cervical, thoracic, and abdominal parts. It has three anatomical constrictions and is supplied by various arteries, veins, and nerves, with clinical relevance to conditions such as esophageal varices and gastroesophageal reflux. Normal functions include swallowing mechanisms and peristalsis, while various abnormalities and diseases can impact its structure and function.