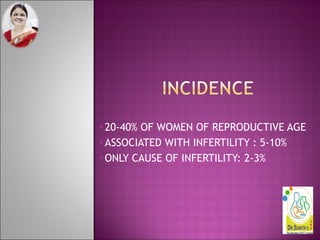
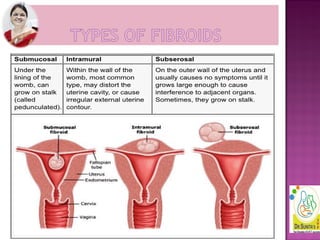
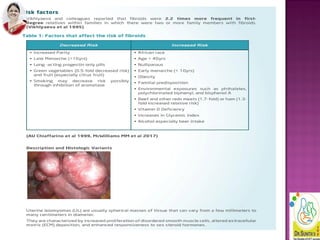
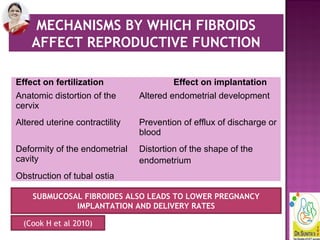
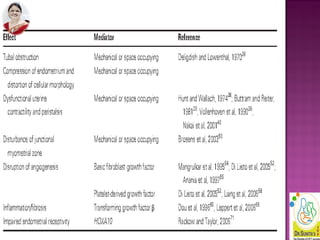
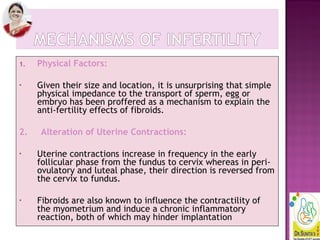
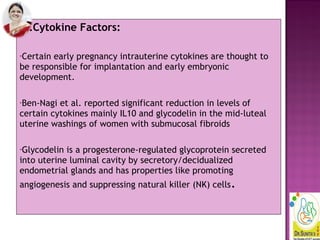
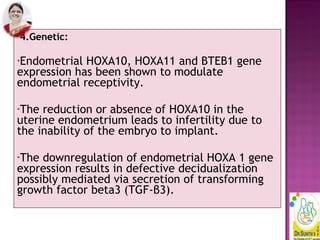
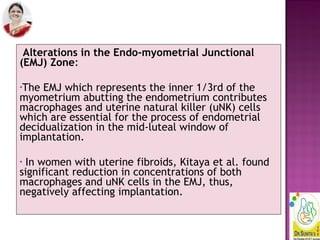
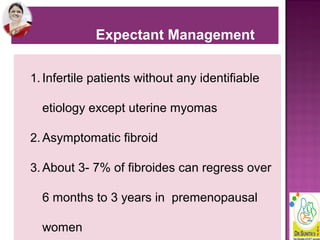
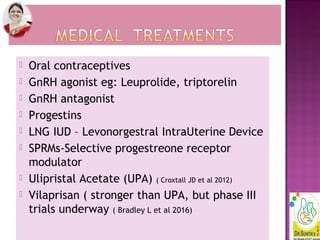
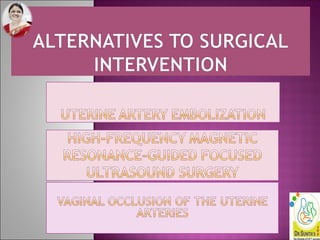
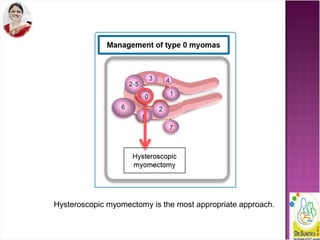
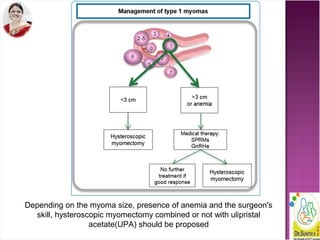
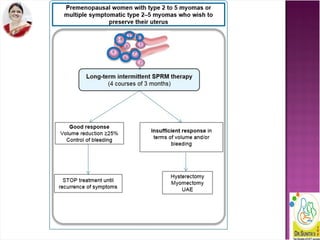
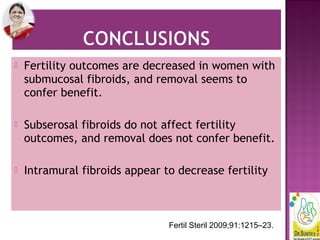
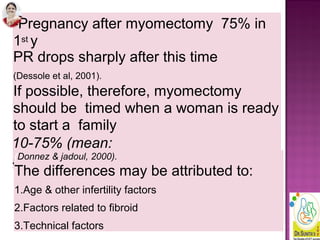
Dr. Sunita Chandra discusses the impact of uterine fibroids on fertility, highlighting that while they affect a significant number of women, most do not influence fertility negatively. Only specific types, such as submucosal and certain intramural fibroids, may require surgical intervention to improve reproductive outcomes. Management options vary based on fibroid characteristics, patient age, and reproductive plans, with a focus on individualized assessment and treatment strategies.