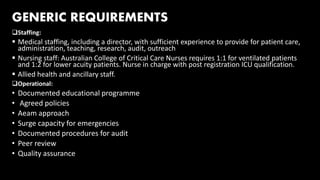
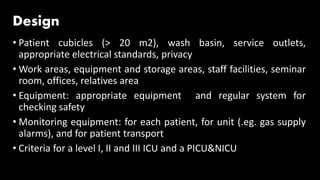
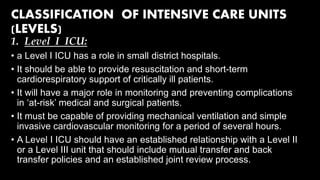
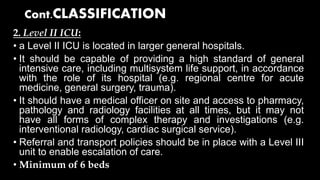
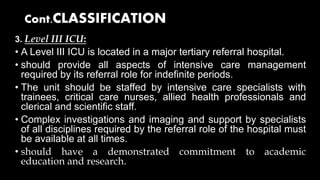
The document defines intensive care units and outlines their staffing, operational, and design requirements. It discusses how ICUs are classified into three levels based on their capabilities and resources. Level I ICUs provide basic life support, Level II offer higher levels of care and multisystem support, and Level III are located in major hospitals and can provide all intensive care services. The document also describes different types of specialty ICUs and high-dependency units that provide intermediate levels of care.