The document discusses various refractive errors and eye conditions including:
- Refractive errors like myopia, hyperopia, and astigmatism which cause blurred vision and can be corrected with glasses or contacts.
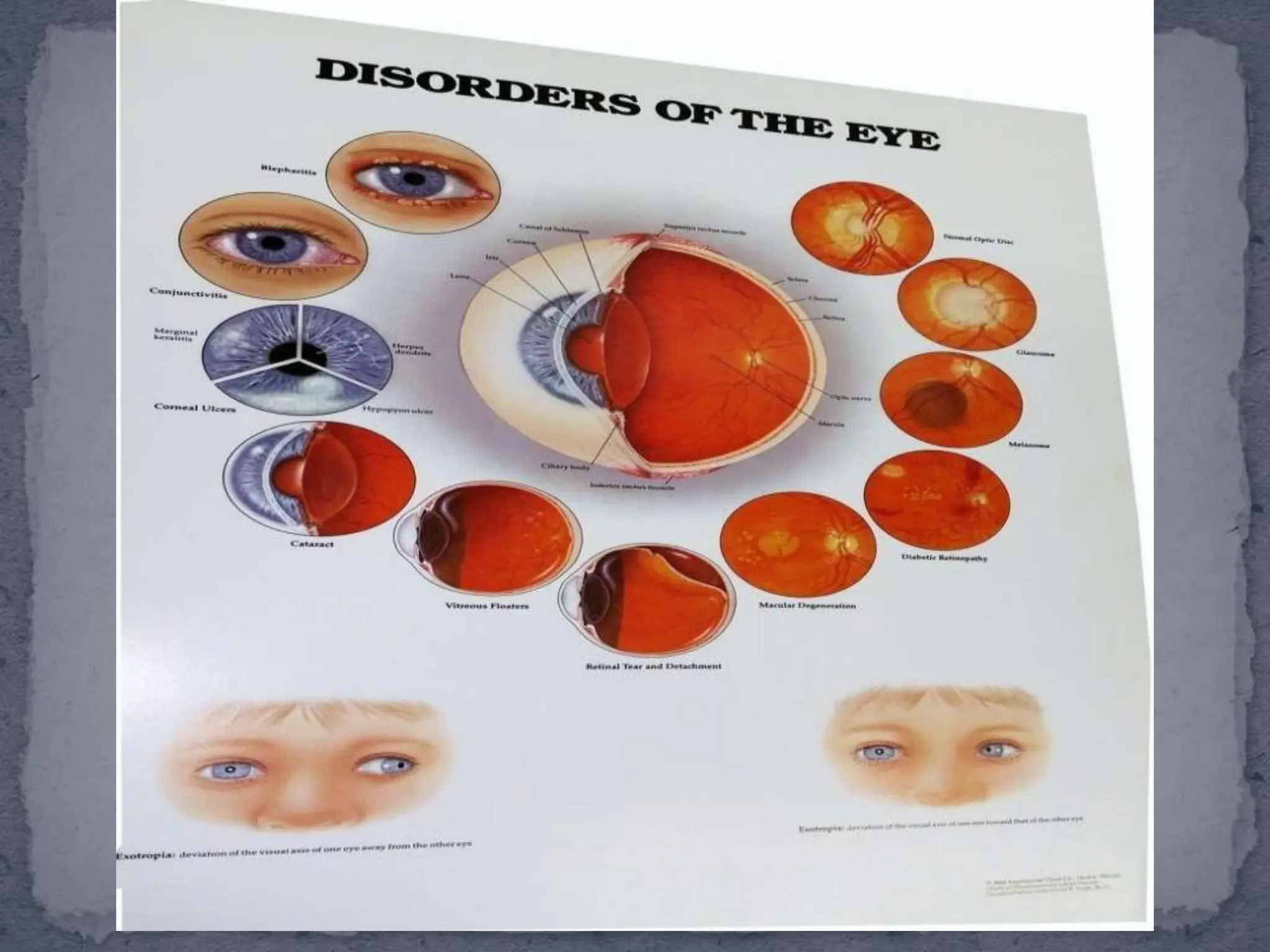
- Eye conditions like strabismus, hordeolum, blepharitis, entropion, and ectropion. Strabismus is eye misalignment while the others involve eyelid inflammation or turning.
- Causes, symptoms, diagnosis, and treatment are described for each condition. Conservative treatments include eyeglasses, contact lenses, warm compresses, and eye drops. Some conditions may require incision and drainage or surgery.