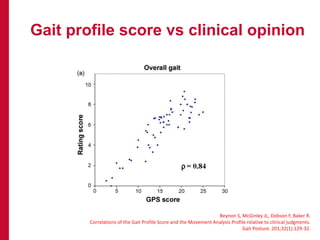
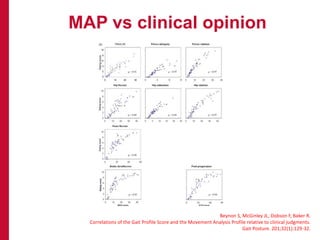
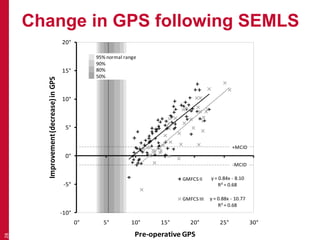
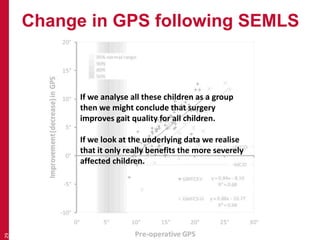
1) Gait analysis provides quantitative measures of walking ability, but the measures need to accurately detect meaningful changes for clinical use.
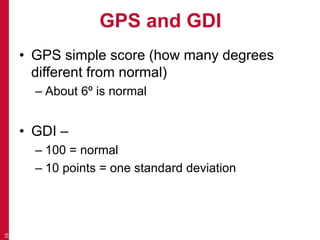
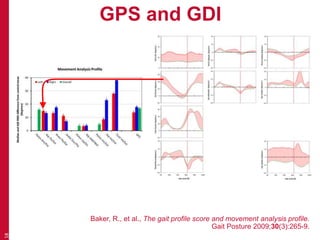
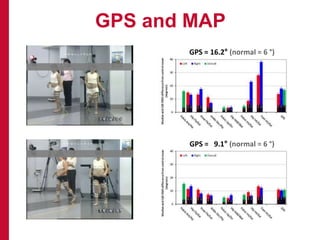
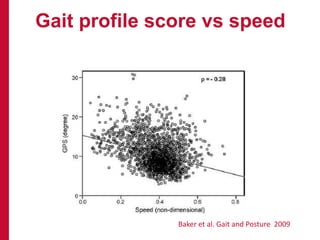
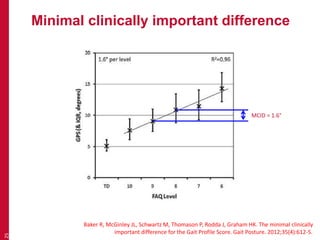
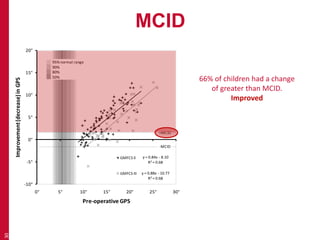
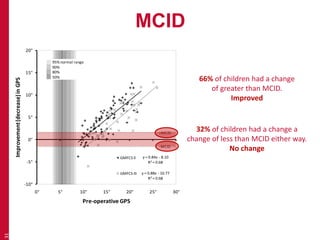
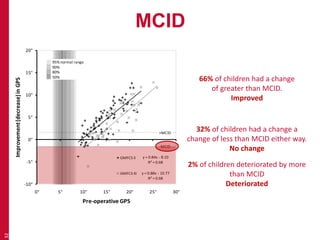
2) The Gait Profile Score (GPS) summarizes overall gait deviation and has a Minimal Clinically Important Difference (MCID) of 1.6 degrees, meaning changes less than this are not noticeable.
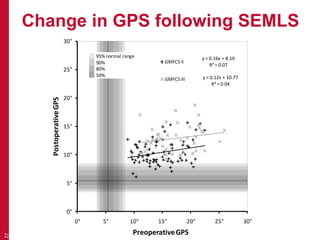
3) An analysis of children who underwent surgery found that 66% improved over the MCID, 32% saw no meaningful change, and 2% deteriorated, showing the ability of GPS to evaluate the effects of interventions.