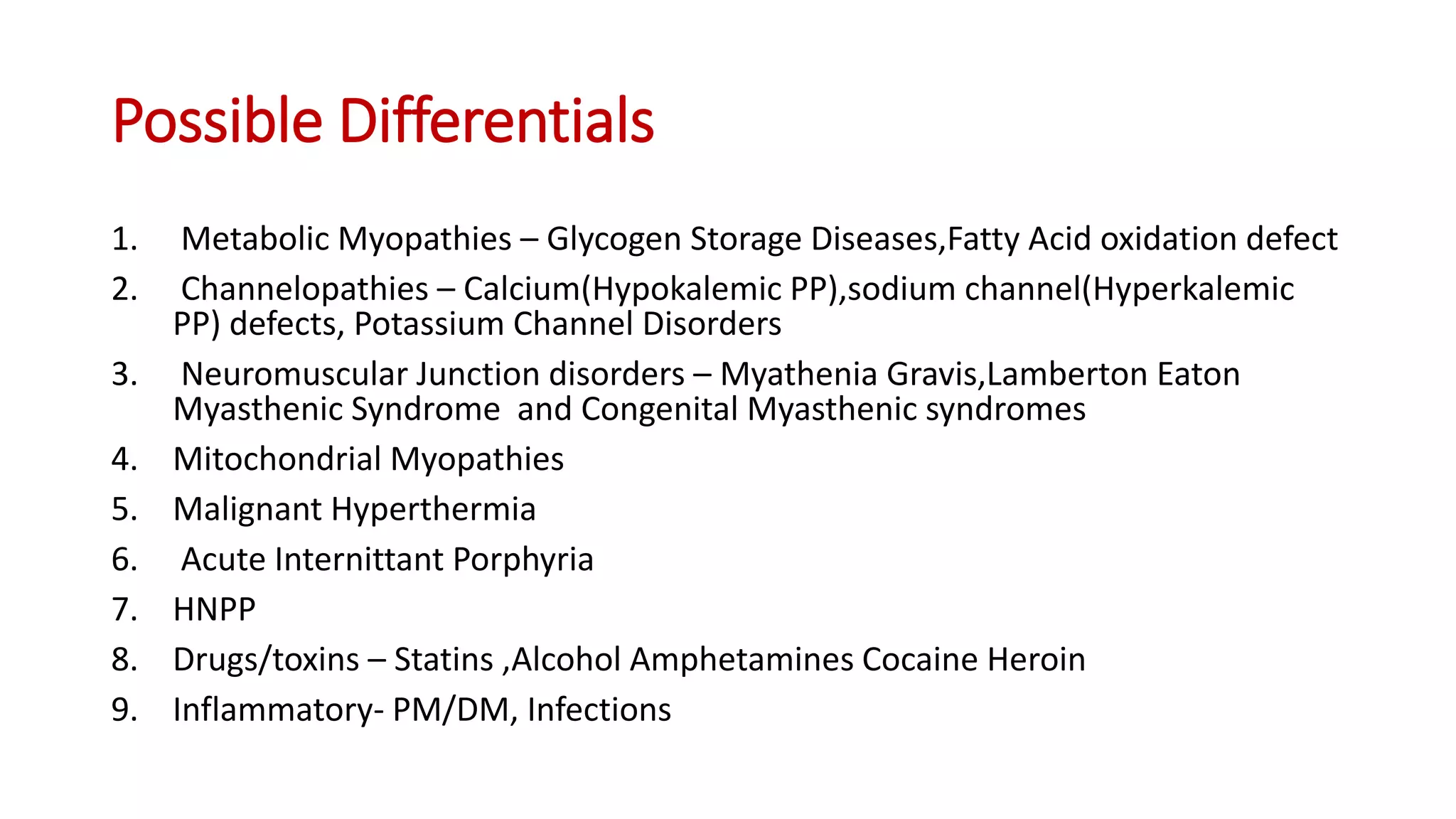
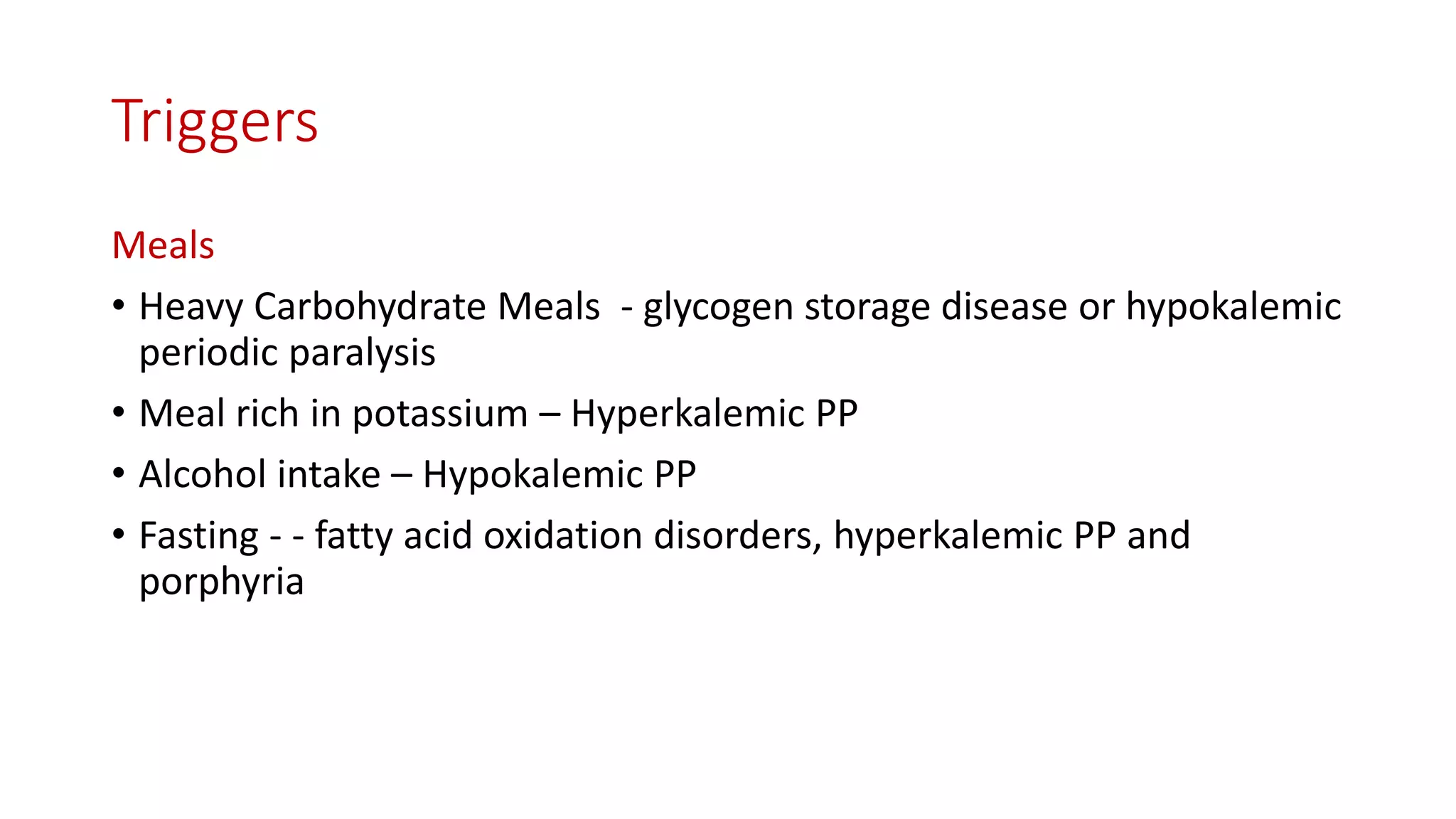
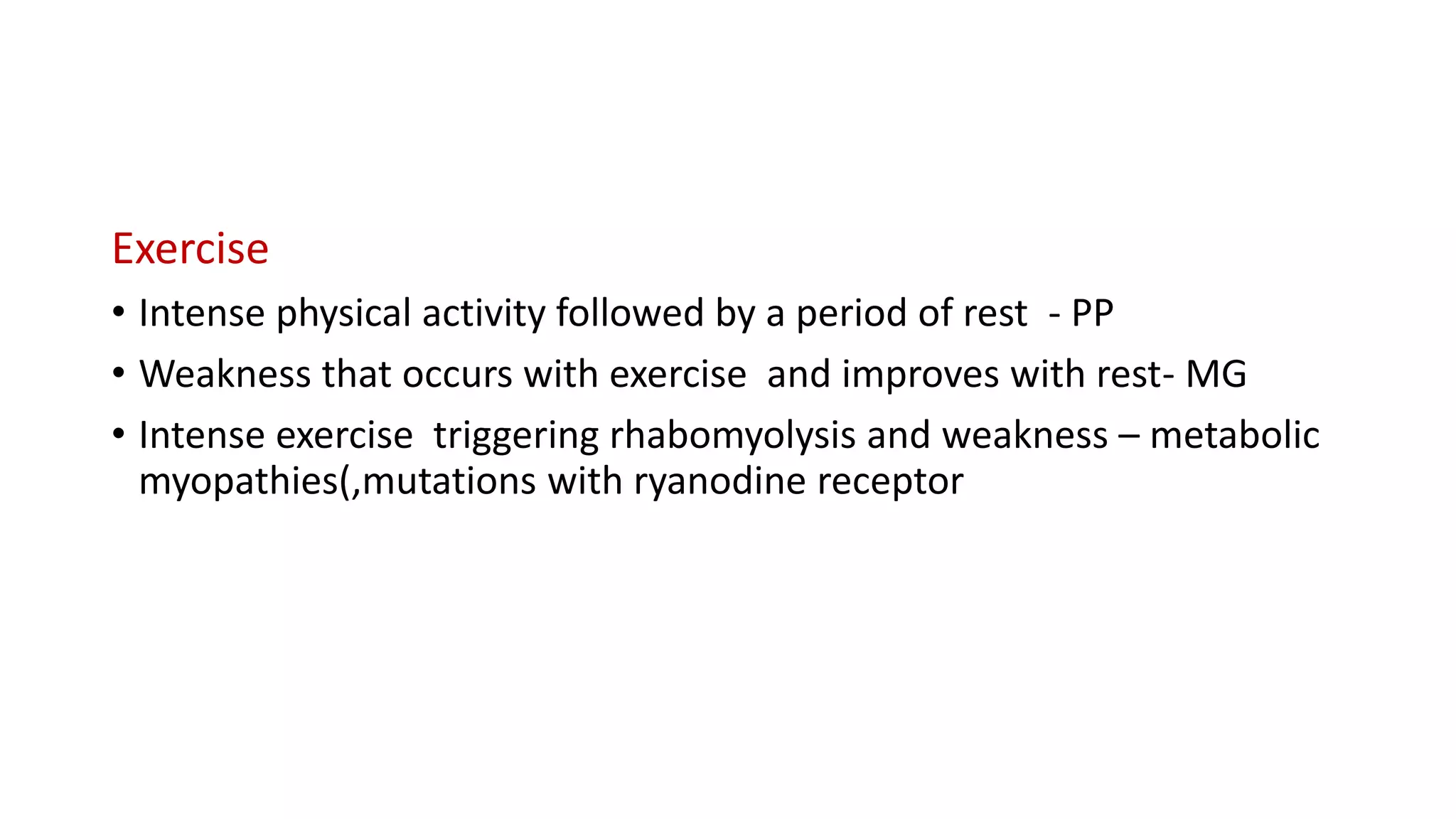
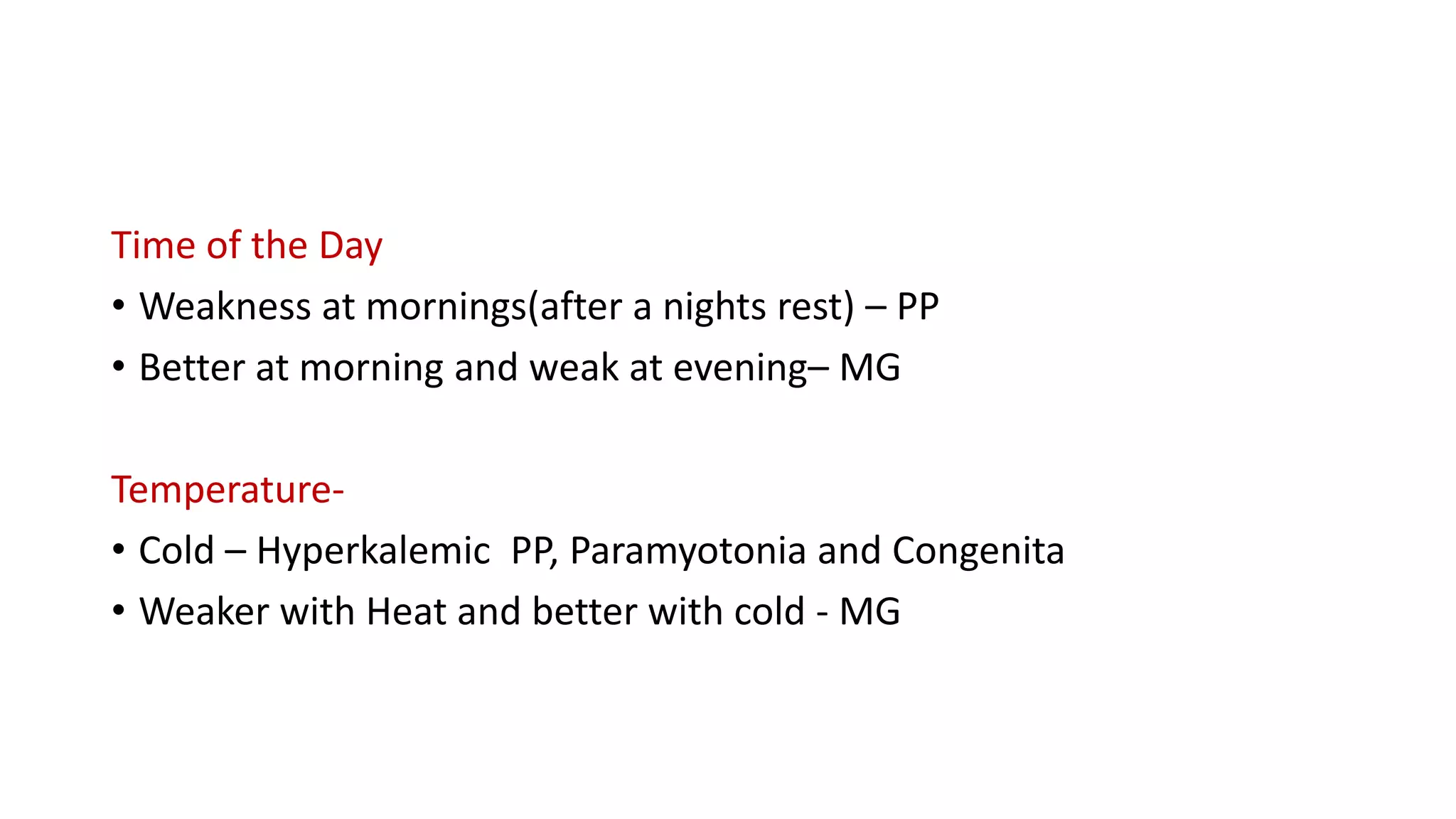
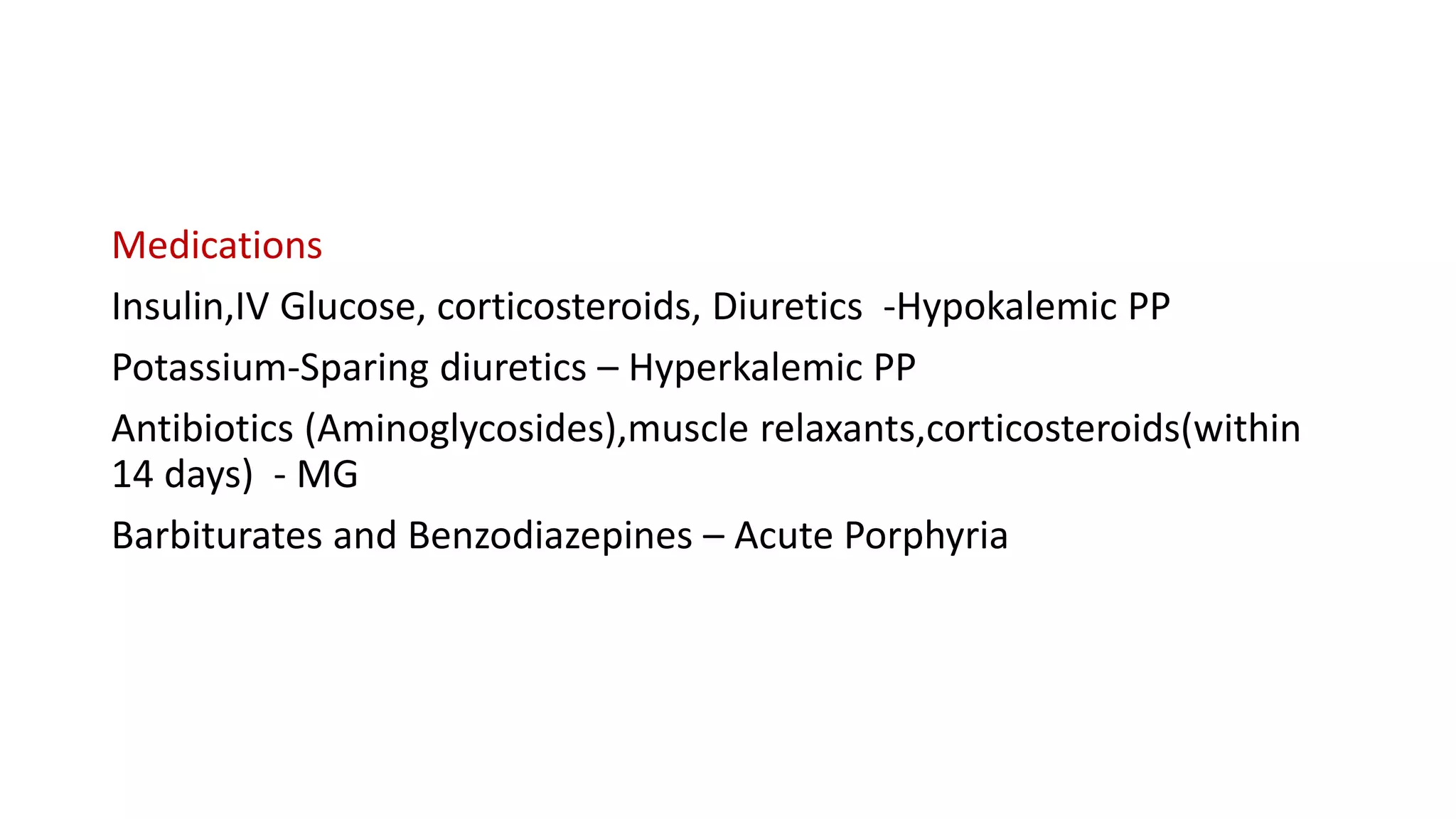
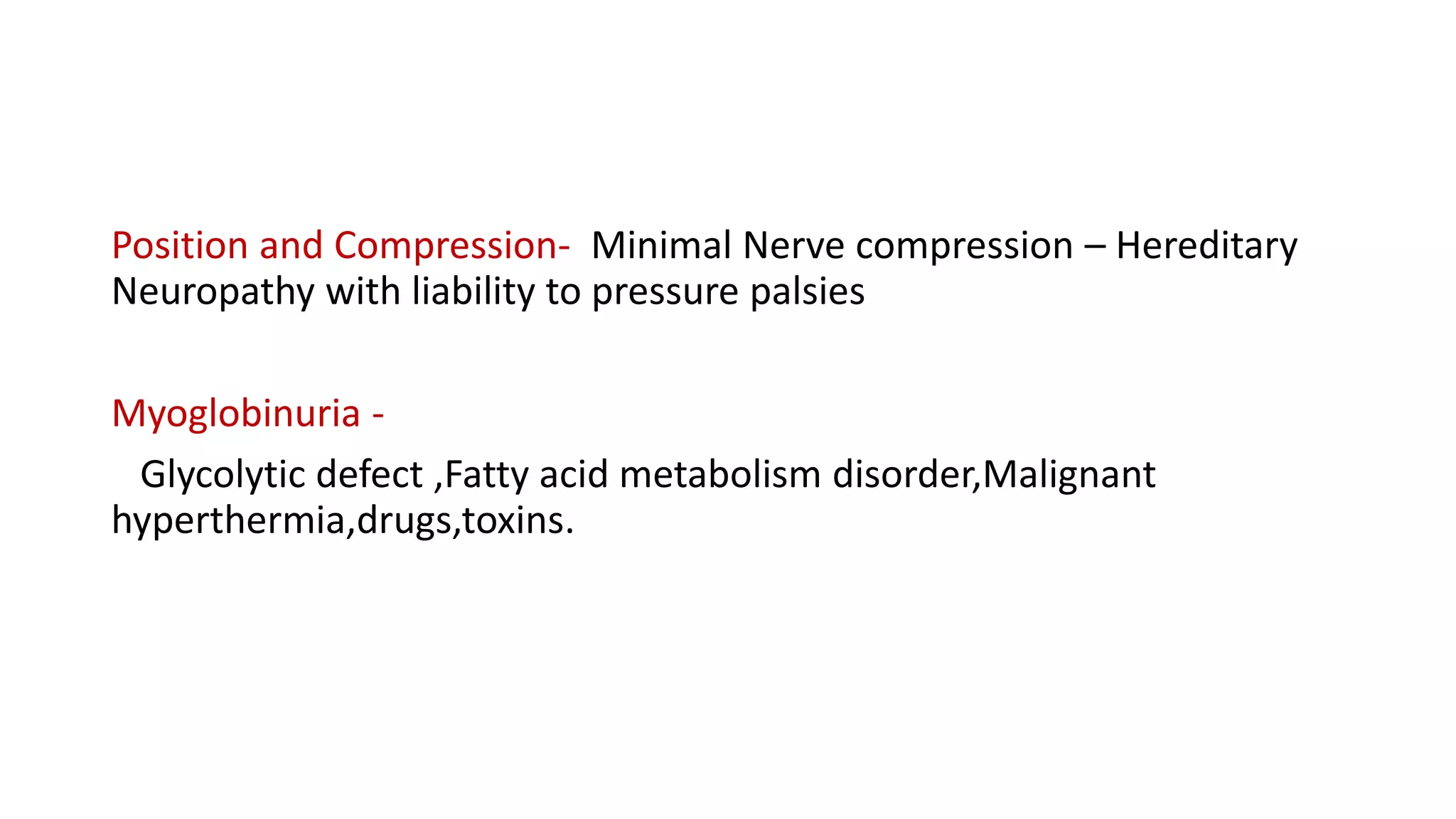
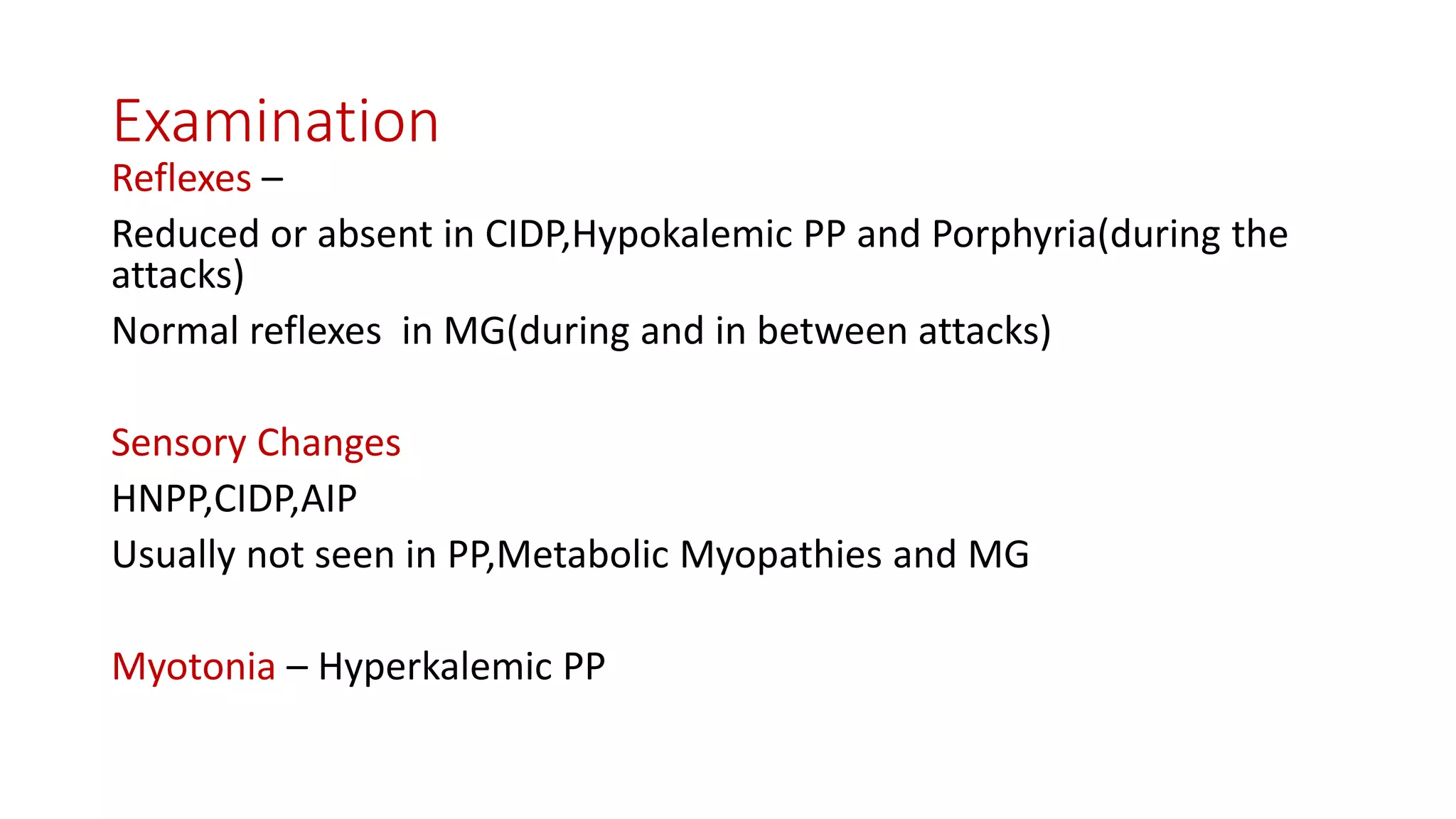
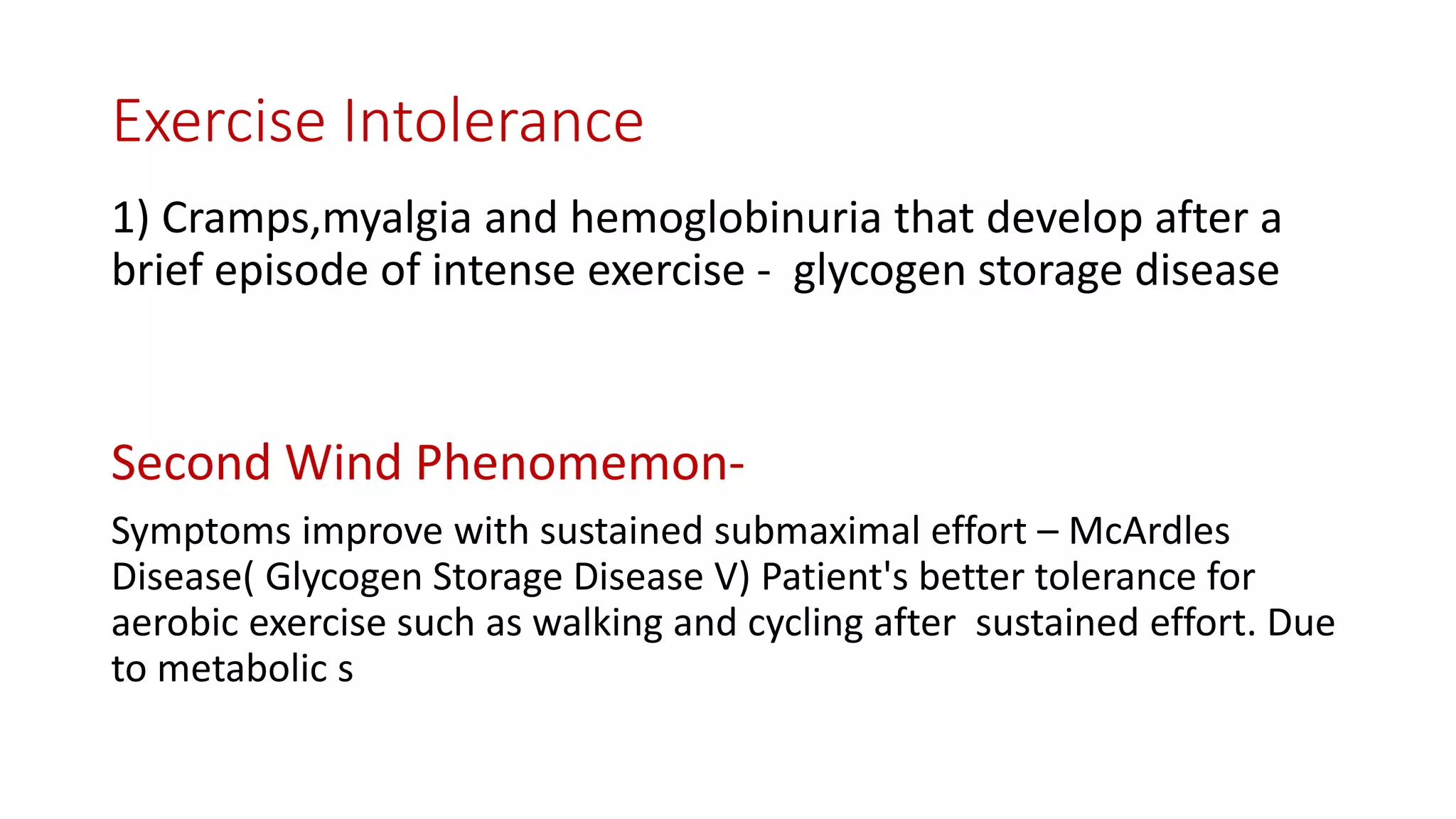
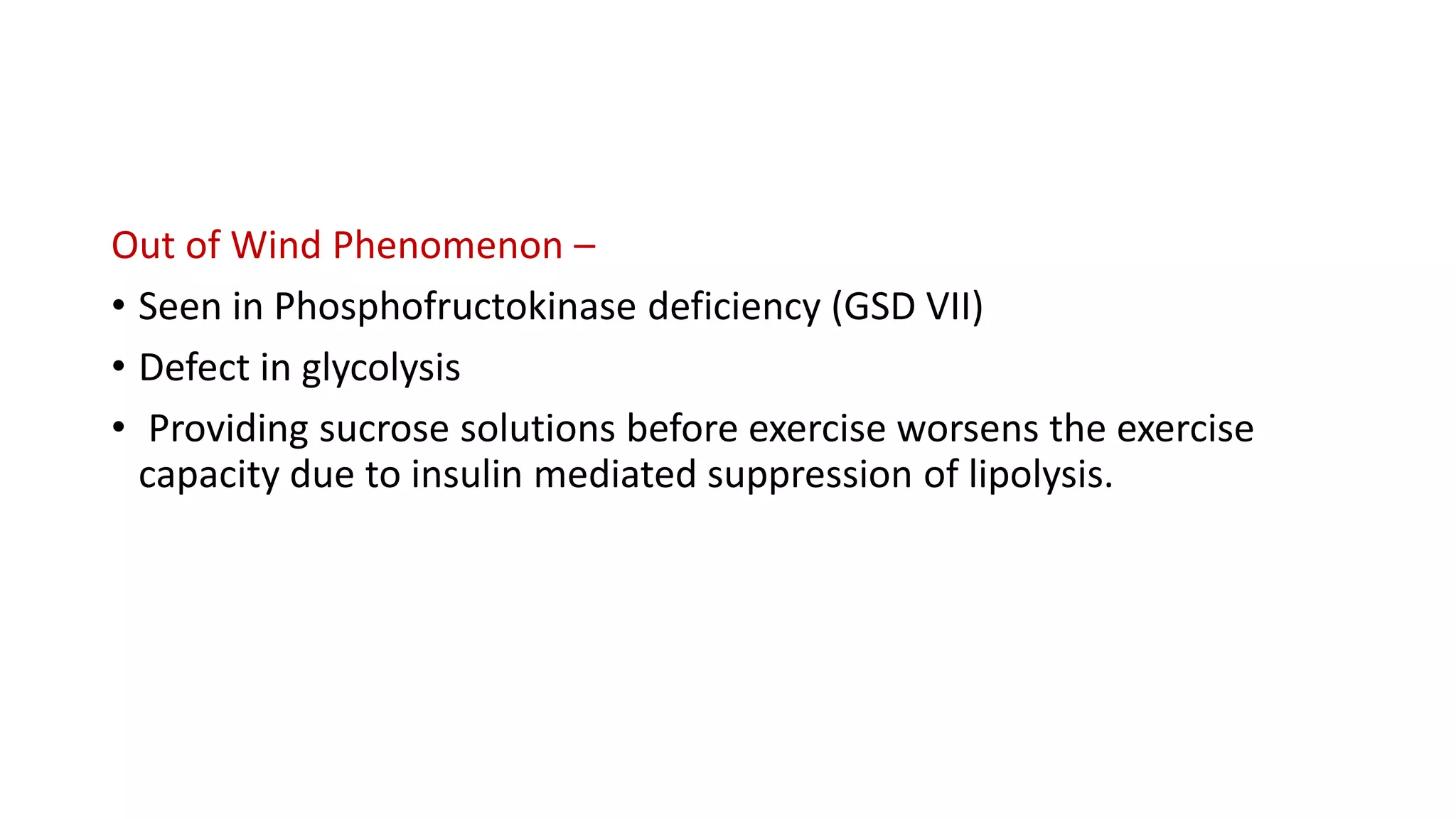
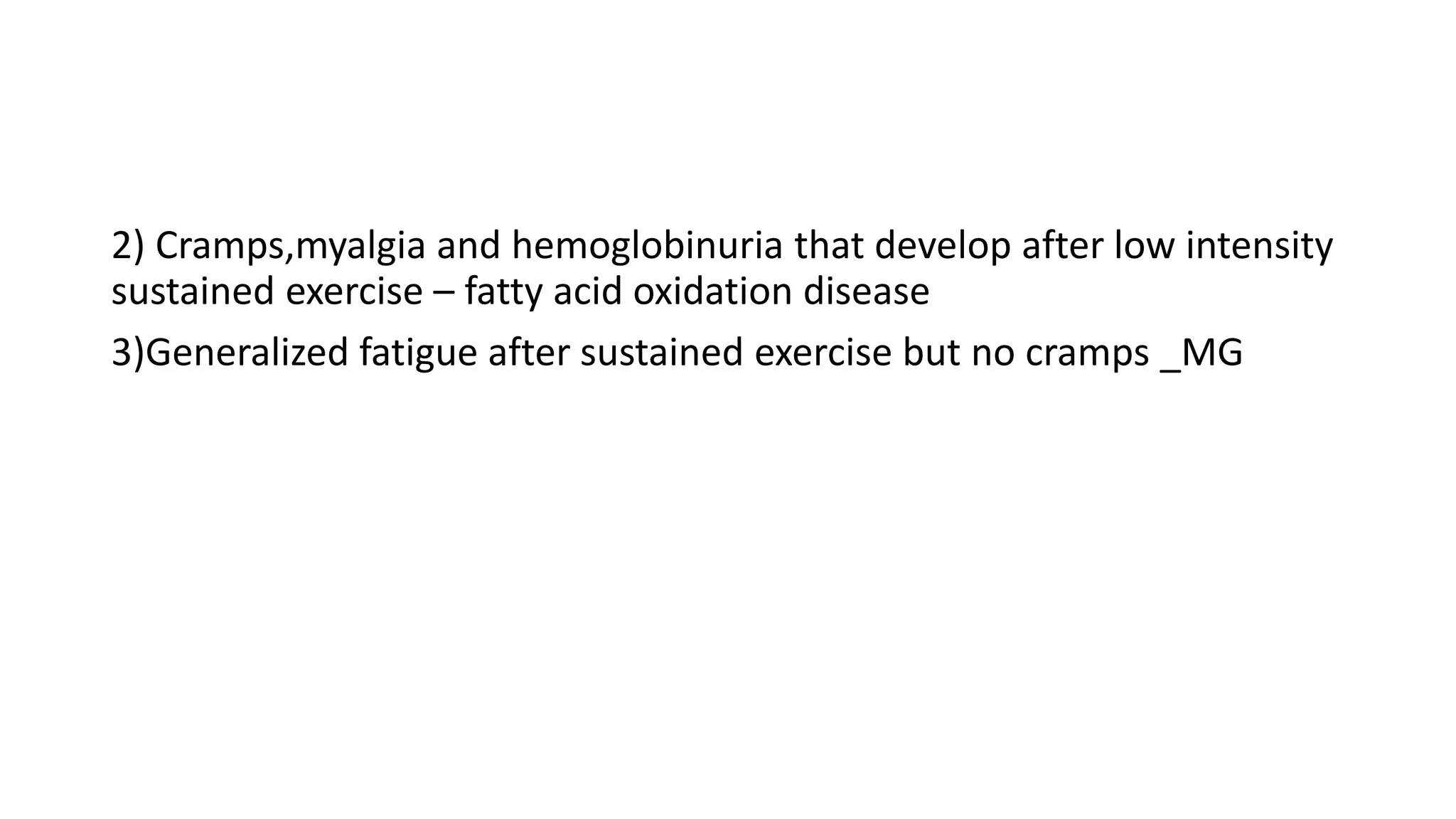
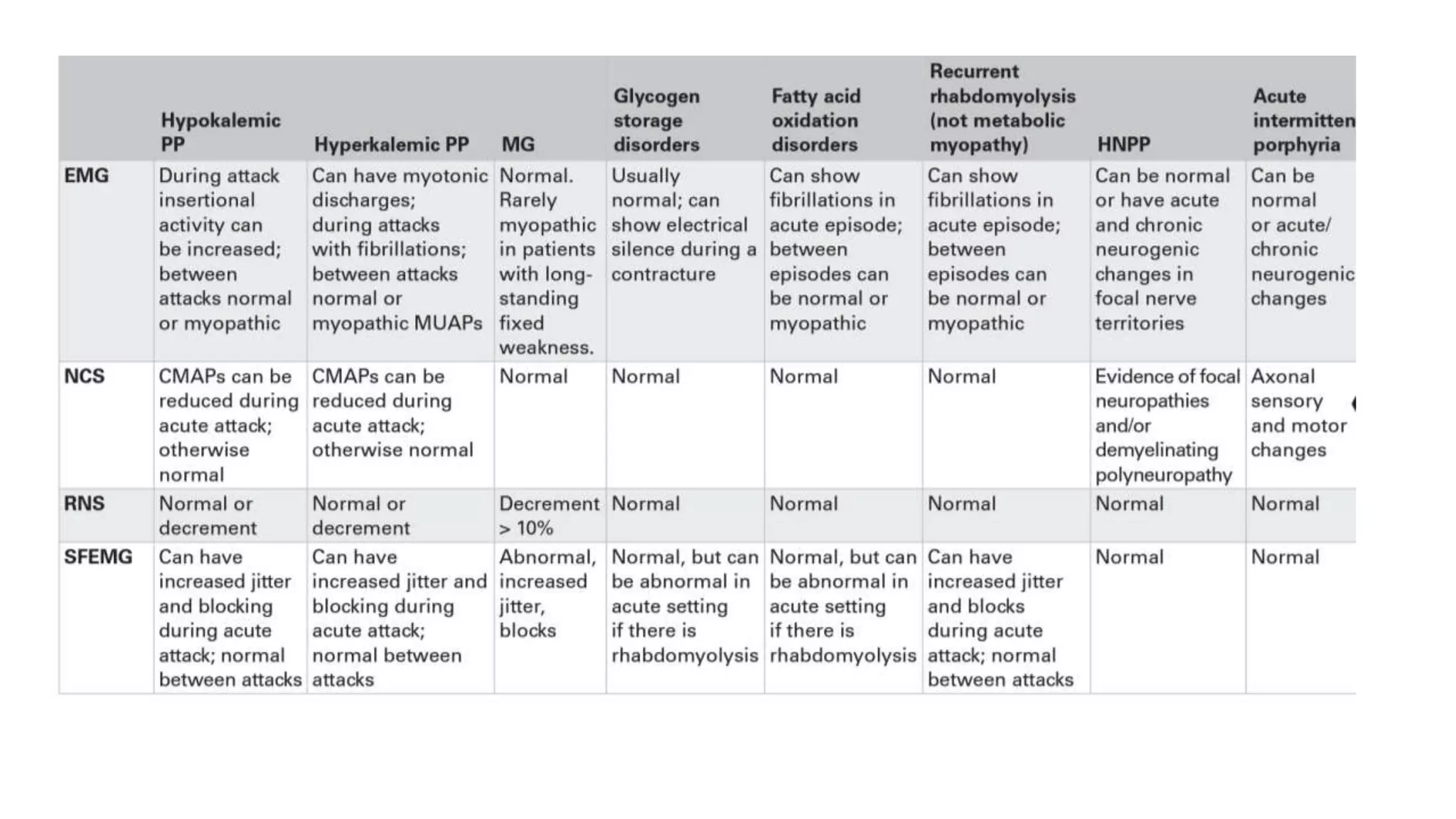
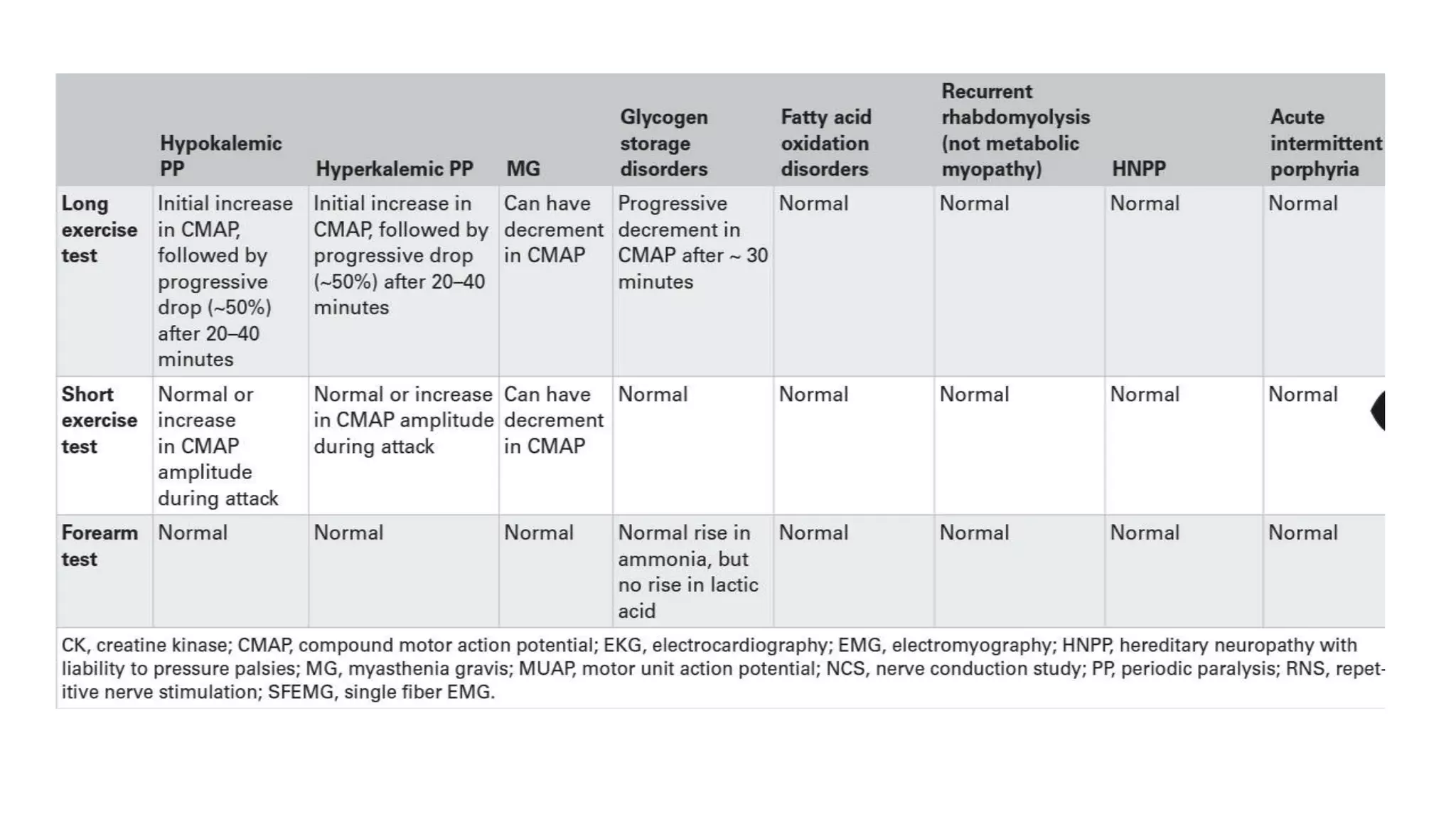
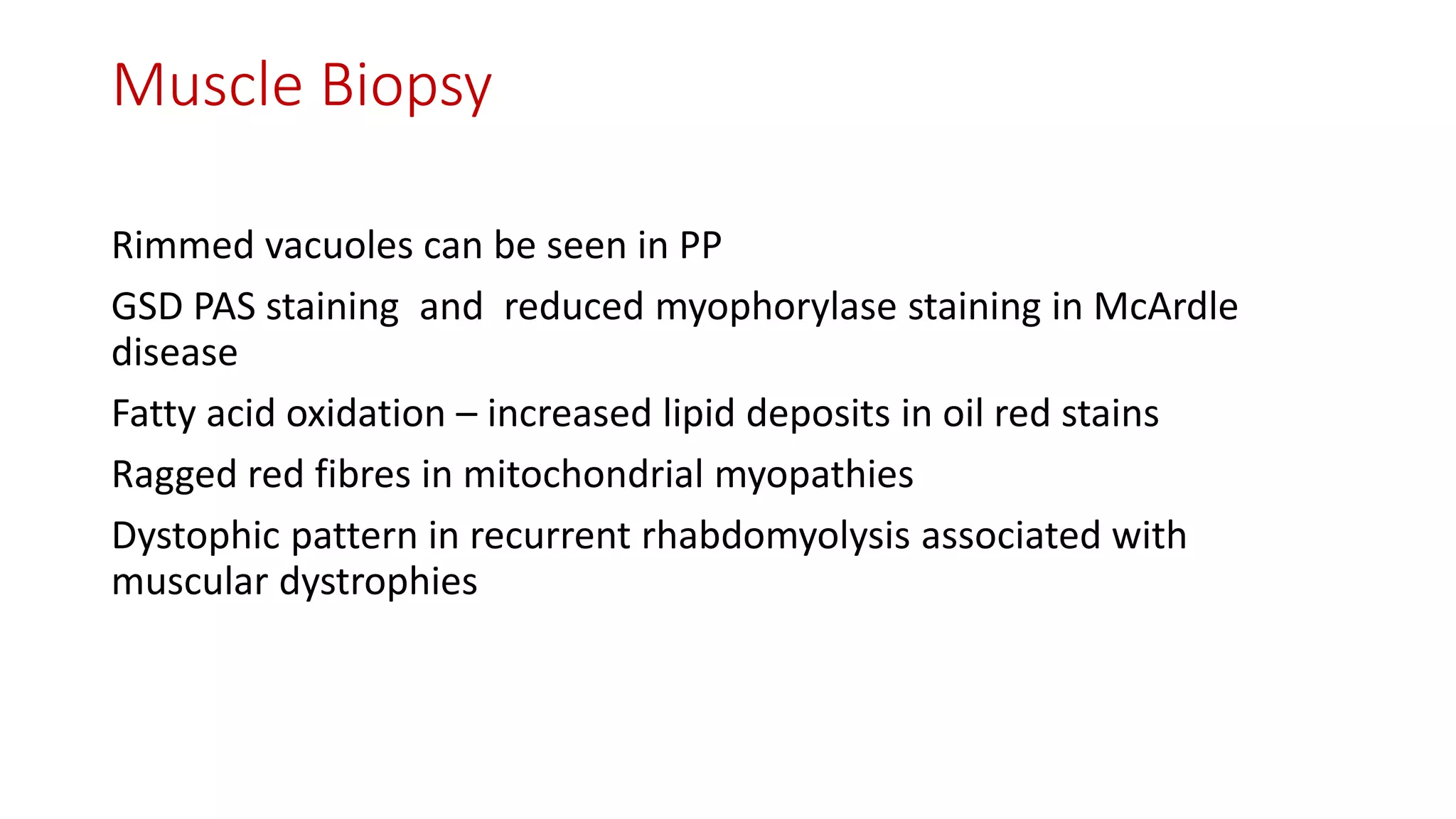
This document discusses the differential diagnosis and approach to evaluating episodic muscle weakness. Potential causes include metabolic myopathies, channelopathies, neuromuscular junction disorders, mitochondrial myopathies, and inflammatory myopathies. The evaluation involves obtaining a detailed history regarding triggers, duration and distribution of weakness, family history, and examination findings. Initial investigations include electrolytes, CK, ECG, pulmonary function tests, and electrodiagnostics. Further testing may include exercise tests, muscle biopsy, and genetic testing to identify specific causes. A systematic approach is required to diagnose the underlying condition causing episodic muscle weakness.