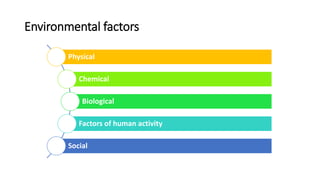
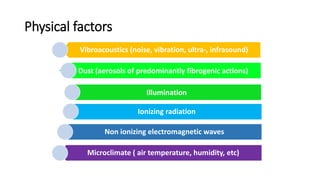
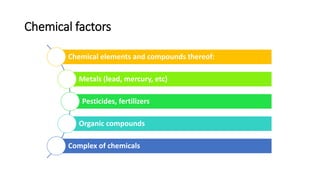
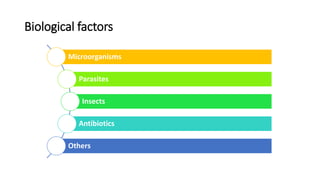
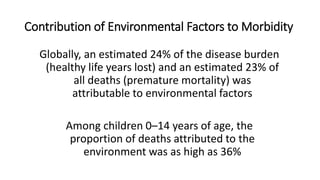
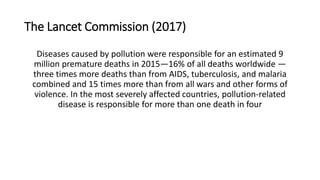
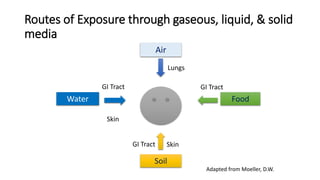
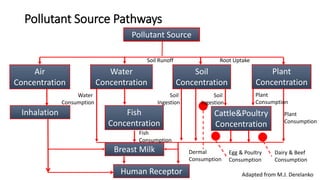
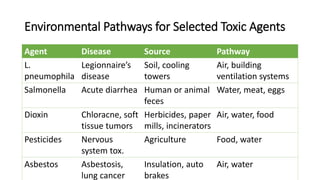
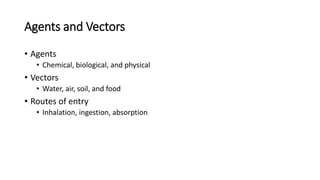
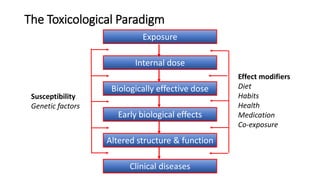
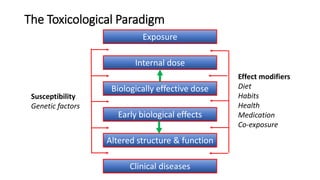
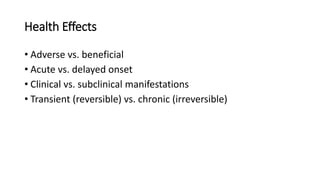
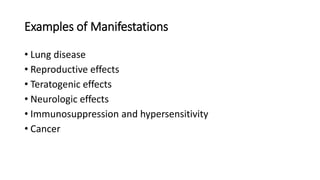
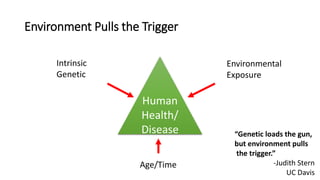
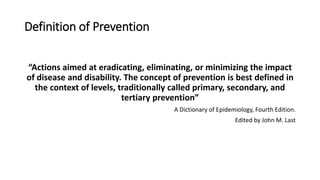
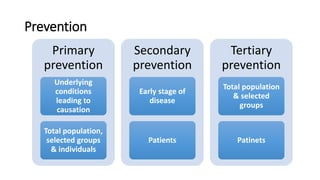
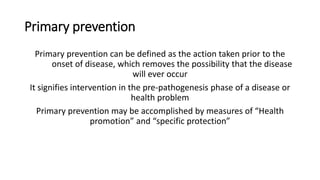
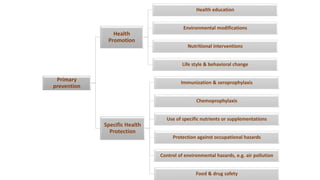
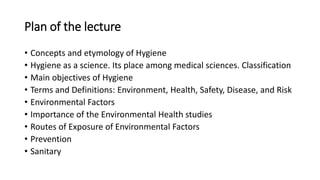
The document discusses environmental hygiene and environmental health. It defines key terms like hygiene, environment, health, disease, and risk. It outlines the main objectives and classification of environmental health science. It discusses the importance of studying environmental factors and their routes of exposure. It also explains concepts of prevention at the primary, secondary and tertiary levels, with a focus on primary prevention measures like health promotion and specific protection.
![Public Health Definition of “The Environment”
All that which is external to the individual host. [It] can be divided into
physical, biological, social, and cultural factors, any or all of which can
influence health status in populations.
−Last, J. M. (Ed.). (1995). A Dictionary of Epidemiology(3rd ed.). New York: Oxford
University Press.](https://image.slidesharecdn.com/ghlec-1-201024153302/85/Environmental-Hygiene-10-320.jpg)