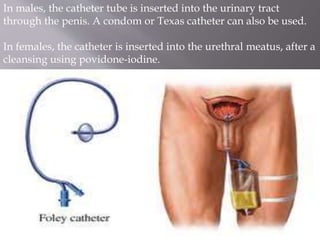
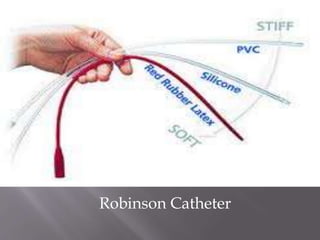
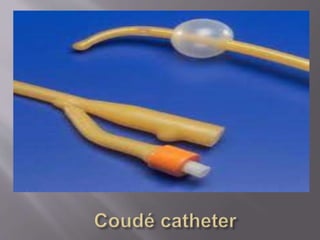
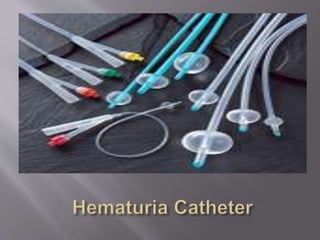
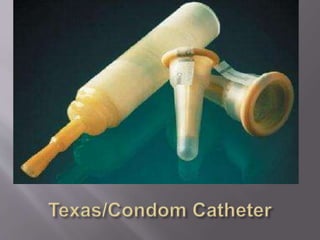
This document discusses urinary catheterization. It describes catheters as plastic tubes inserted into the bladder via the urethra to drain urine or inject liquids for treatment or diagnosis. Critically ill patients requiring strict urine output monitoring are often catheterized. The document describes different catheter types including Foley, Robinson, Coude, and hematuria catheters.