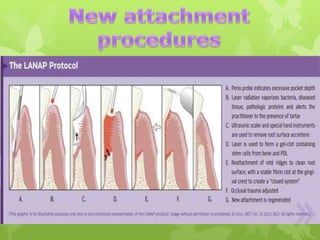
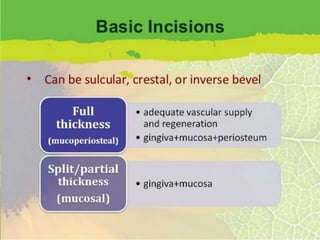
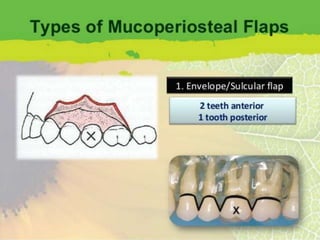
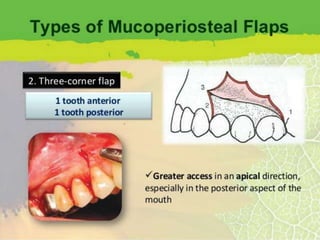
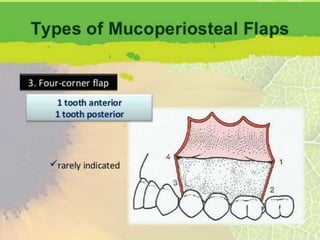
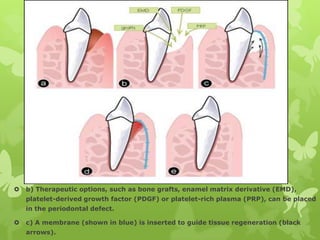
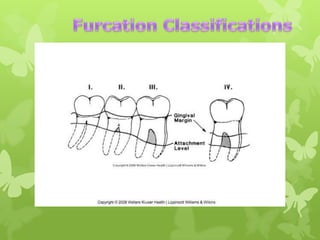
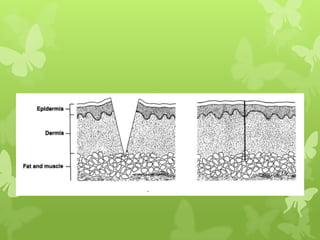
The document discusses various surgical procedures in periodontics and dentistry. It covers indications for surgery such as deep pockets or furcation involvement. It describes resective, regenerative, and new attachment procedures. Regenerative procedures use grafts, EMD, PDGF or PRP with membranes to guide tissue regeneration. Post-operative instructions and complications are addressed. Healing by first, second or third intention is summarized.