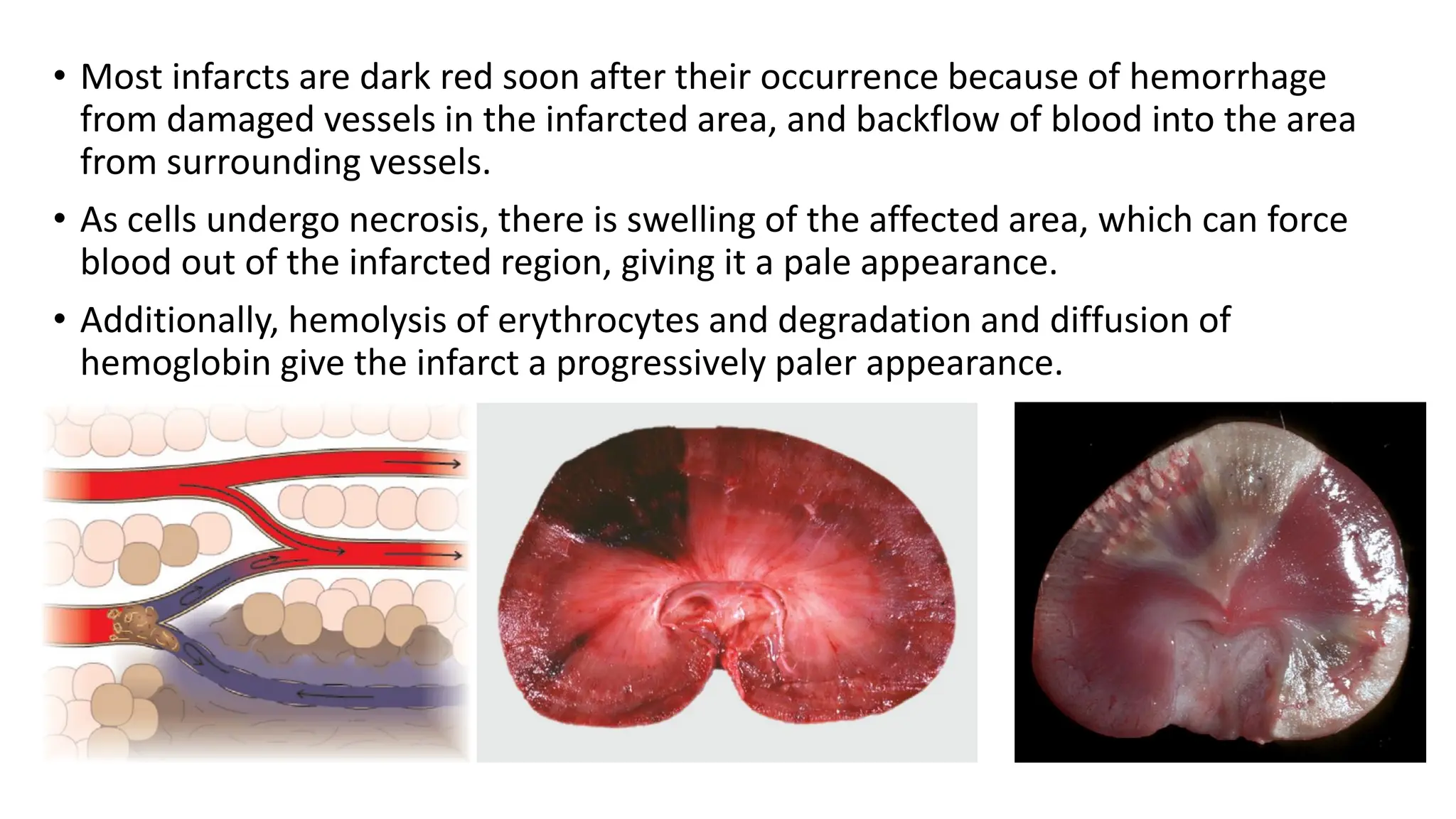
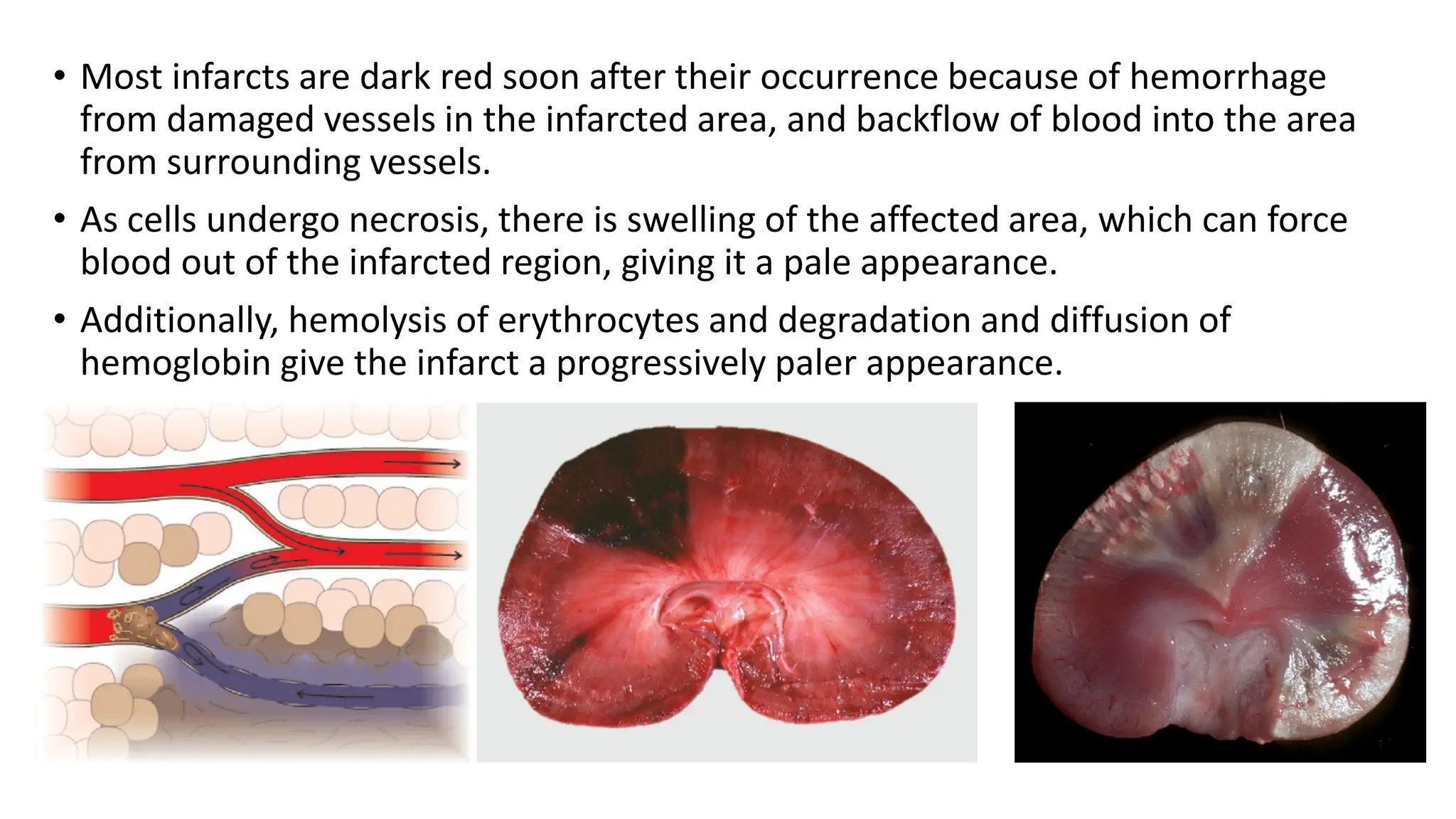
Ischemia occurs when blood flow to tissue is insufficient to meet metabolic needs, often due to arterial blockage or venous obstruction, leading to tissue damage. Infarction, a severe form of ischemia, results in coagulative necrosis and is influenced by factors such as vascular supply and tissue susceptibility to hypoxia. Infarcts are characterized as hemorrhagic or anemic based on blood accumulation, with varying appearances depending on the blood supply and nature of obstruction.