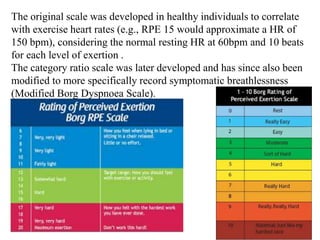
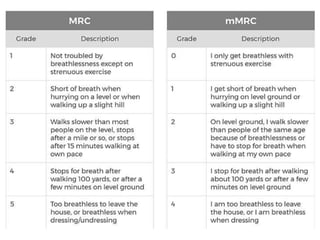
The document discusses scales used to measure dyspnea in patients with chronic respiratory diseases. It describes the Borg scale and modified Borg dyspnea scale, which allow patients to subjectively rate their level of exertion. It also describes the mMRC dyspnea scale, which measures perceived respiratory disability by having patients indicate how breathlessness affects their mobility. These scales are useful for clinicians to quantify dyspnea, describe disability levels, and assess changes after treatment. Pulmonary rehabilitation can help reduce dyspnea through various mechanisms like improving muscle function, reducing ventilatory impedance, and decreasing central drive.