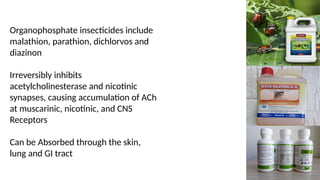
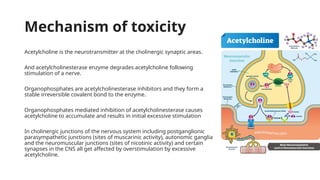
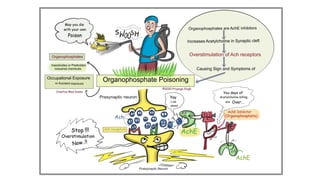
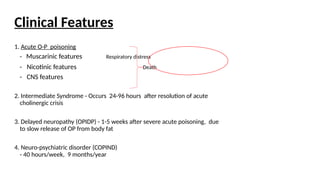
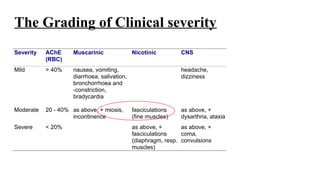
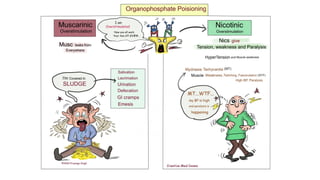
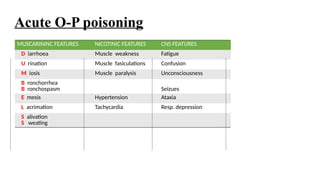
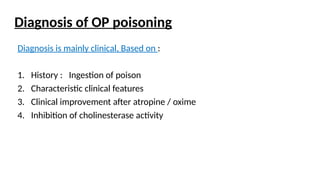
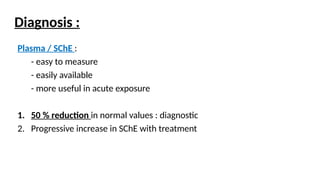
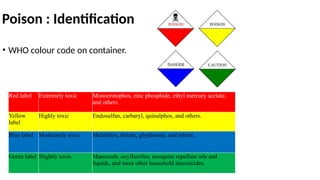
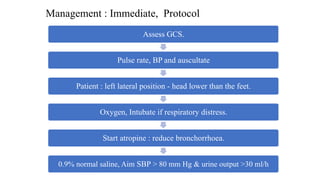
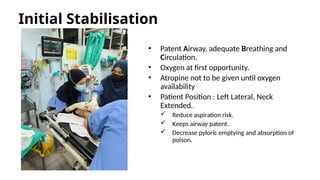
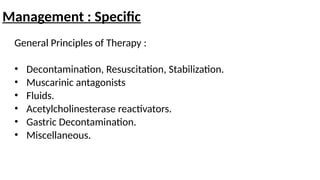
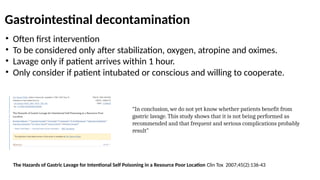
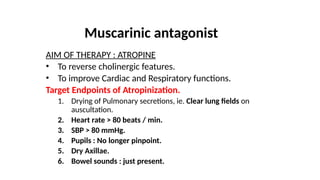
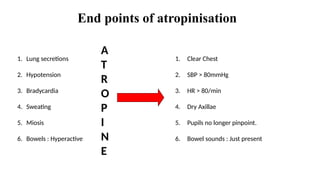
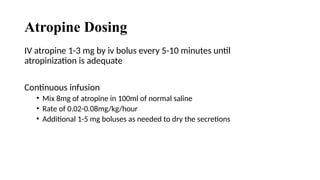
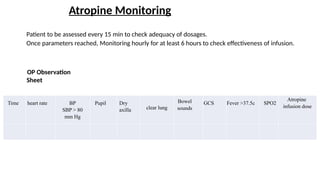
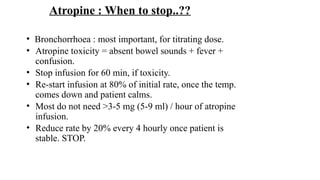
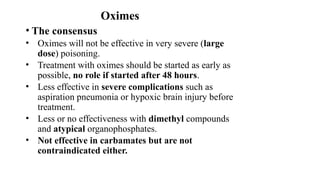
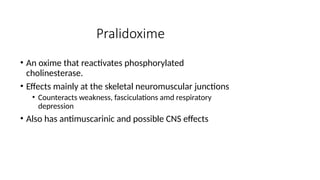
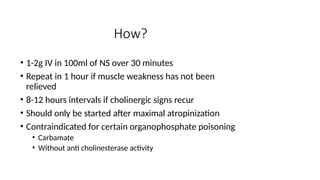
The document outlines the mechanisms of organophosphate (OP) poisoning, highlighting that OP insecticides irreversibly inhibit acetylcholinesterase, resulting in the accumulation of acetylcholine and subsequent cholinergic symptoms. It further discusses the clinical features, diagnosis, and management protocols, including the use of atropine and oximes to counteract poisoning effects. The increase in pesticide poisoning incidents in Malaysia is also noted, particularly among younger male adults, emphasizing the need for better education and access control.