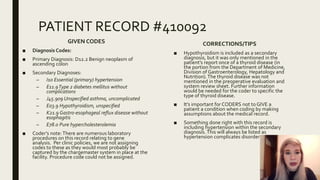
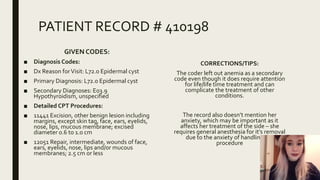
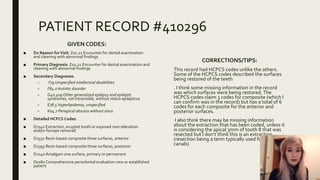
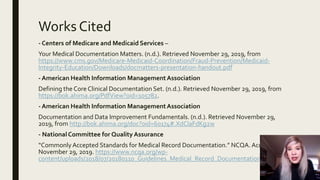
The document discusses the importance of proper clinical documentation for patient care, reimbursement, and communication. It notes that accurate, complete documentation is a shared goal for all healthcare workers. An internal audit is recommended to check documentation completeness and identify areas for improvement. Examples of incomplete or inaccurate patient records are provided and analyzed to illustrate documentation best practices. Maintaining proper documentation requires understanding guidelines and including all relevant clinical information.

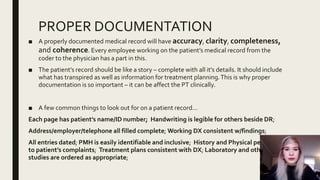

![PATIENT RECORD #410057
CODES GIVEN:
■ Diagnosis Codes:
■ Dx Reason forVisit: C50.411 Malignant neoplasm of
upper outer quadrant of right female breast
■ Primary Diagnosis: C50.411 Malignant neoplasm of
upper outer quadrant of right female breast
■ Secondary Diagnosis: Z17.1 Estrogen receptor
negative status [ER-]
■ Detailed CPT Procedures:
■ 19301-RT Partial Mastectomy; (RT Right side of
body)
■ 14301 Adjnt tis trnsfr/reargmt any area 30.160 sq
cm
■ 19285-RT Placement of breast localization
device(s), percutaneous; first lesion, including
ultrasound guidance; (RT – Right side of the body)
CORRECTIONS/TIPS:
■ For this case, I’m not finding the information
that would cause the coder to select the
secondary diagnosis. I think further
information in the HPI would be needed to
confirm the negative estrogen receptor
status.
■ It’s important for medical necessity to be met
when coding documents and in this case,
there may be additional information needed
that may have been left out somewhere (PMH
or Laboratory Reports) to apply the secondary
diagnosis as on the patient’s record.There is
no clinical mention other than in the
secondary DX of the condition.
■ A good example of documentation would be
the CPT modifiers of “RT” that signify the
patient’s right breast was the one in which the
procedure was performed. It’s important not
to forget these.](https://image.slidesharecdn.com/practiciumpresentation-191205195405/85/Documentation-Improvement-Presentation-5-320.jpg)