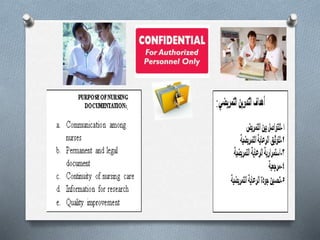
1) Documentation and charting are integral parts of a nurse's responsibility to advocate for patients and defend nursing actions through demonstrating the standard of care was provided.
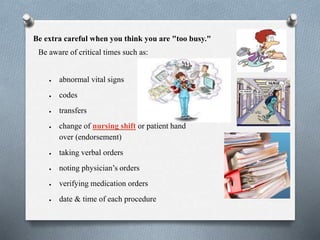
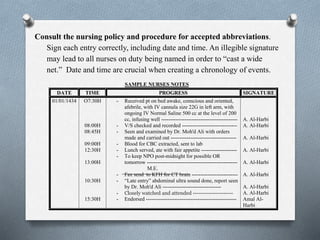
2) Nurses must be careful to document critical times such as abnormal vital signs, codes, transfers, and changes of shift, as well as noting orders, procedures, and assessments.
3) Late entries, corrections, and "too perfect" charting can raise doubts, so nurses should follow policy on documentation and use clear, specific language without abbreviations in their notes.