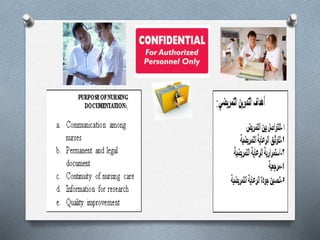
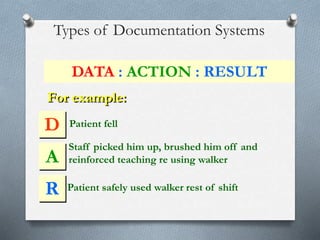
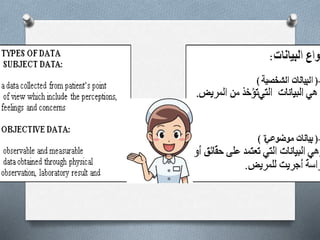
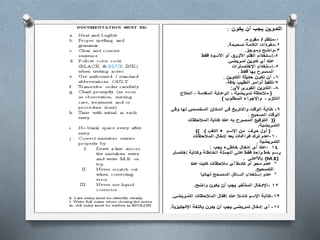
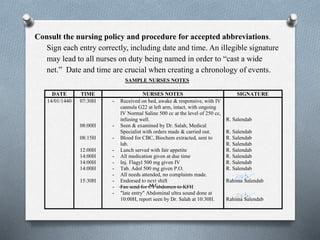
Nursing documentation, also known as charting, is a key part of a nurse's responsibility to advocate for patients and defend their care. It involves recording all assessments, procedures, medications, and other relevant details about a patient's condition and treatment. Poor or missing documentation makes it difficult to demonstrate that appropriate care was provided and standards were met. Nurses must follow documentation policies, record details accurately and legibly, and avoid vague statements to ensure their charting clearly represents the care delivered to each patient.