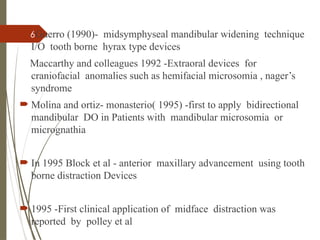
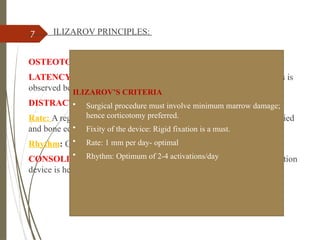
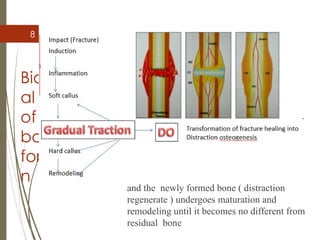
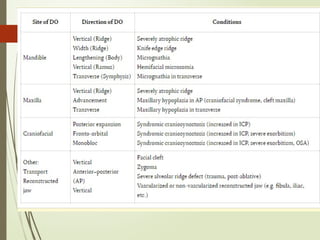
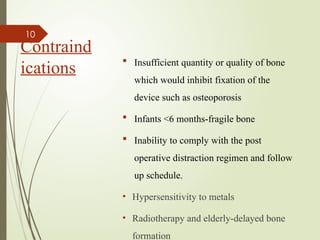
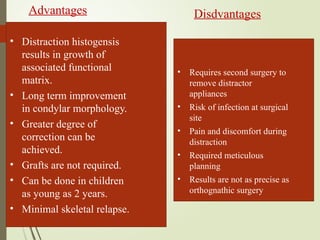
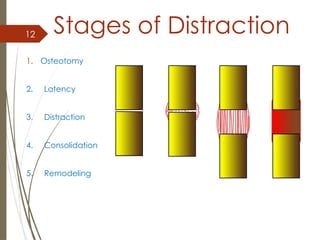
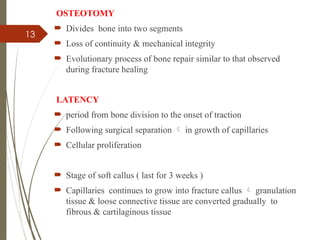
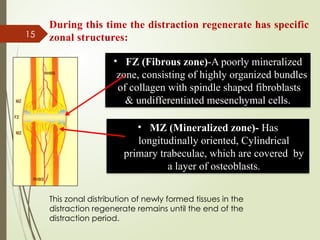
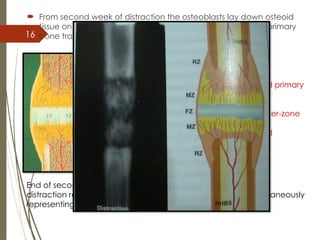
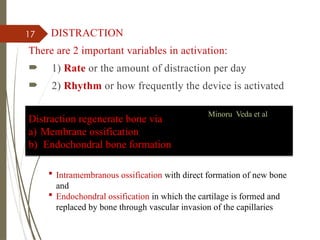
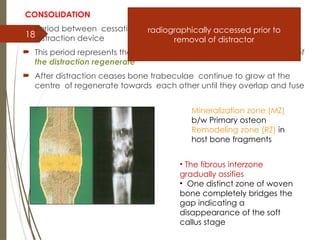
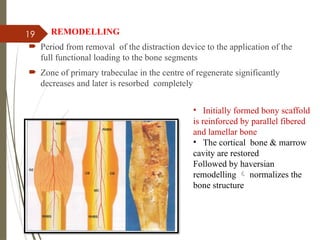
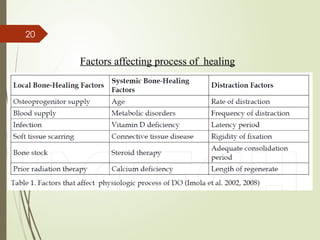
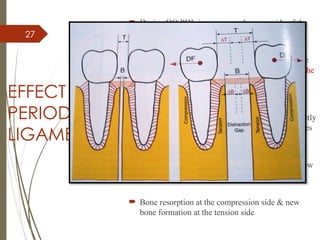
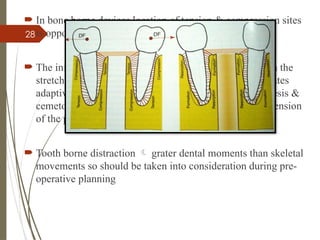
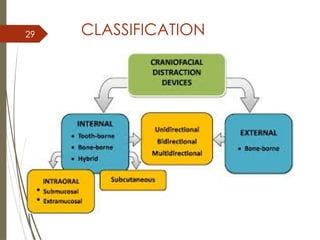
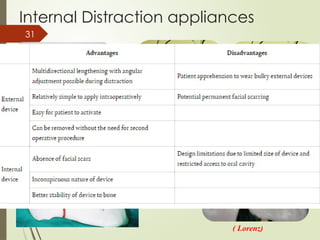
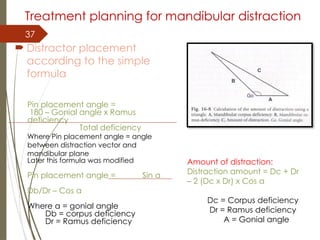
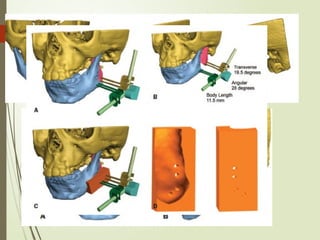
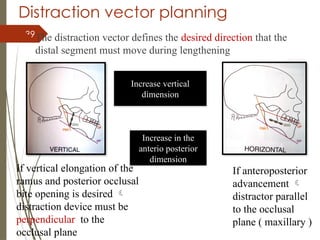
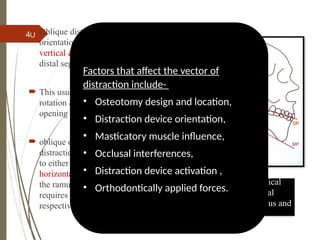
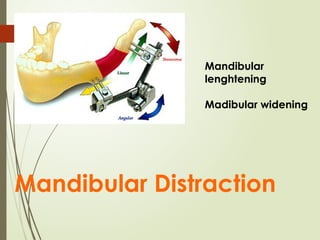
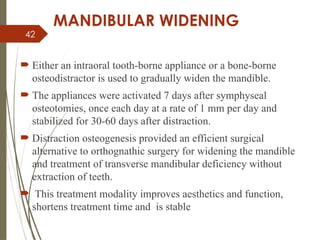
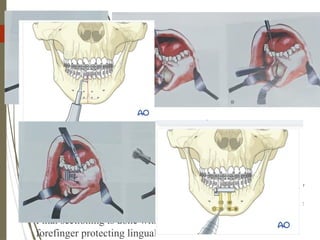
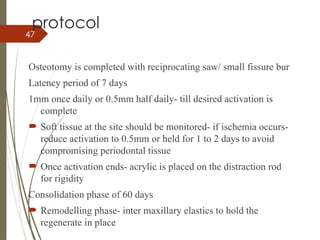
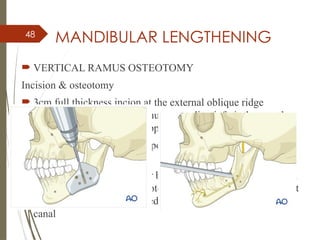
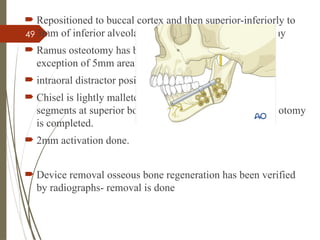
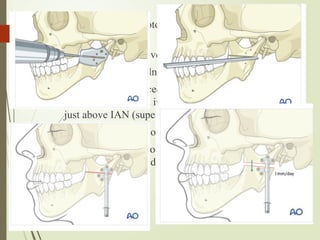
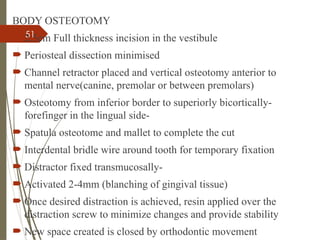
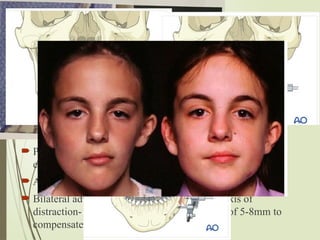
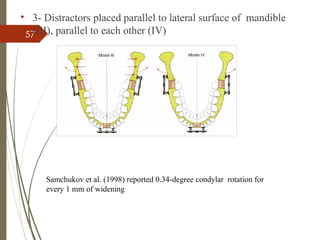
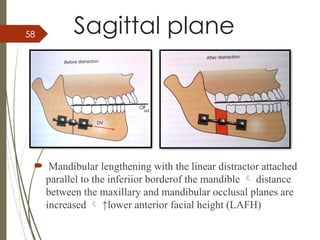
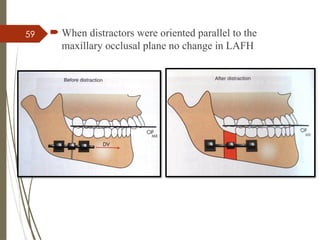
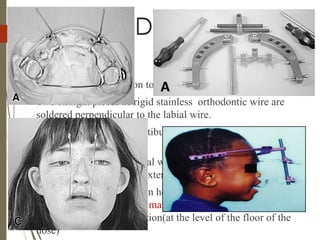
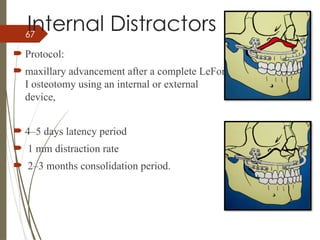
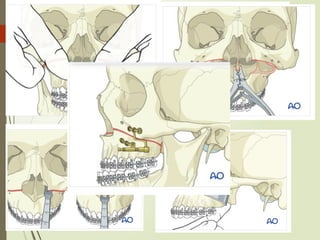
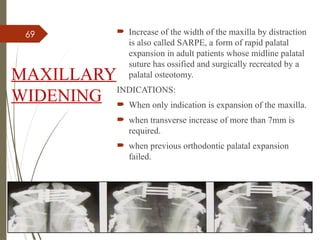
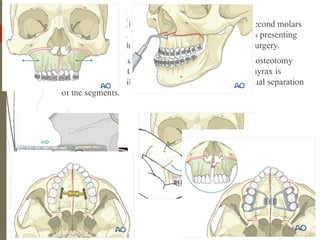
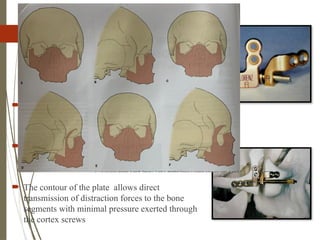
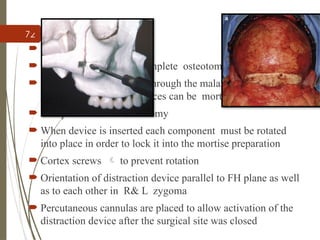
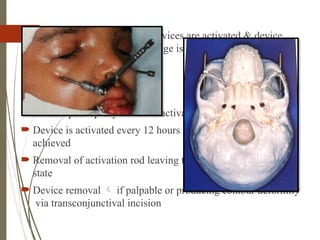
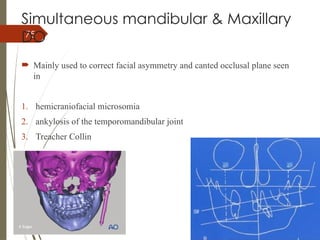
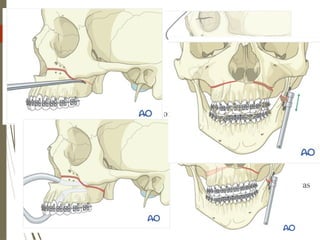
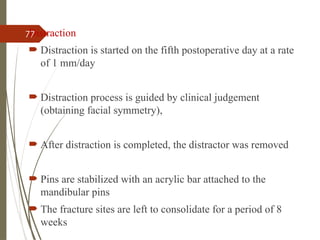
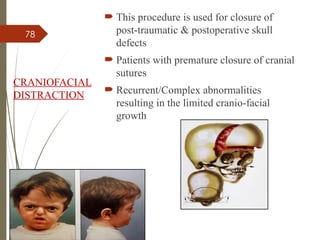
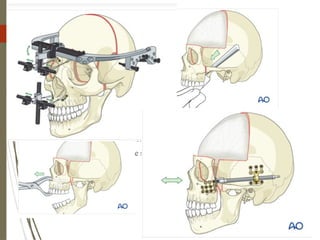
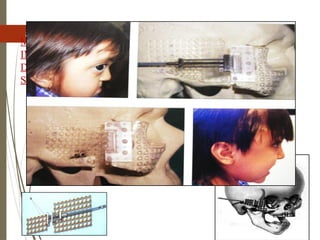
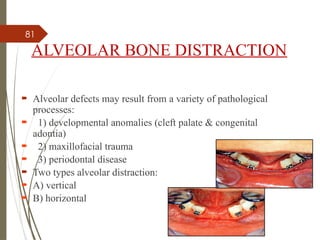
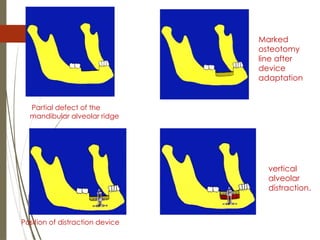
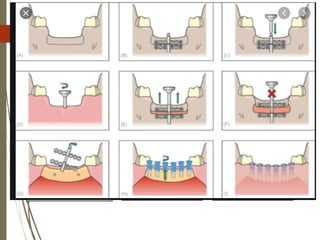
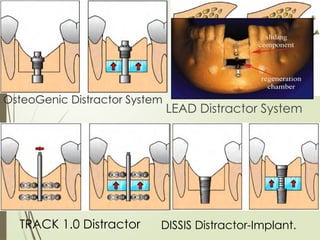
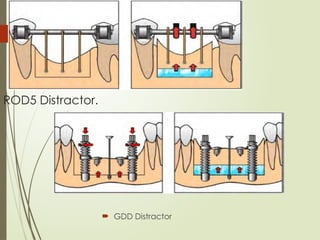
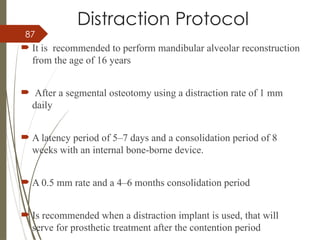
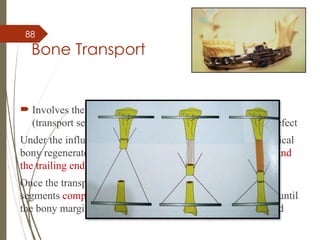
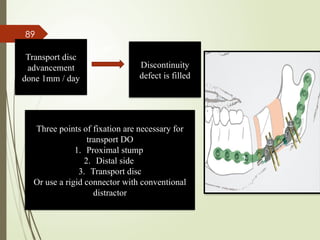
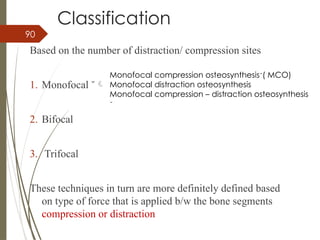
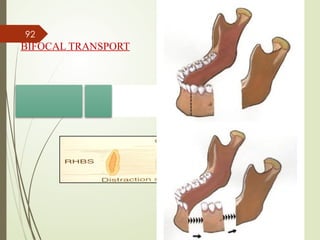
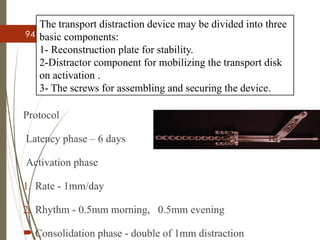
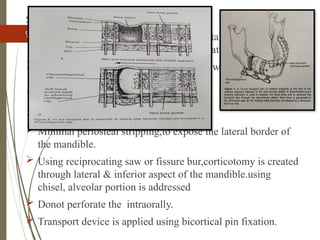
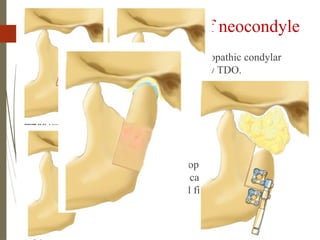
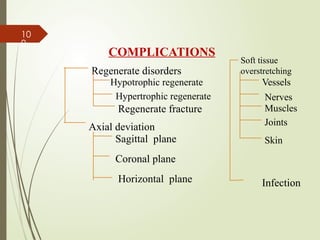
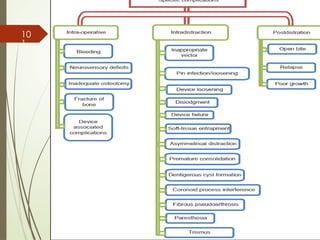
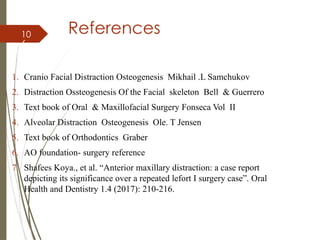
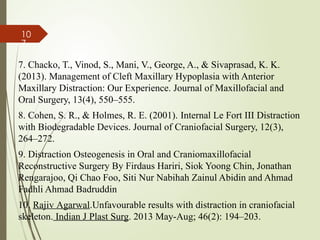
The document presents a comprehensive overview of distraction osteogenesis, describing its definition, historical development, and biological mechanisms that facilitate new bone formation through incremental traction. It discusses various applications, indications, contraindications, advantages, and disadvantages of the technique, as well as the stages of the procedure, including osteotomy, latency, distraction, consolidation, and remodeling. Key contributions from historical figures and principles, such as those introduced by Ilizarov, are elaborated while emphasizing the importance of meticulous planning in clinical applications.