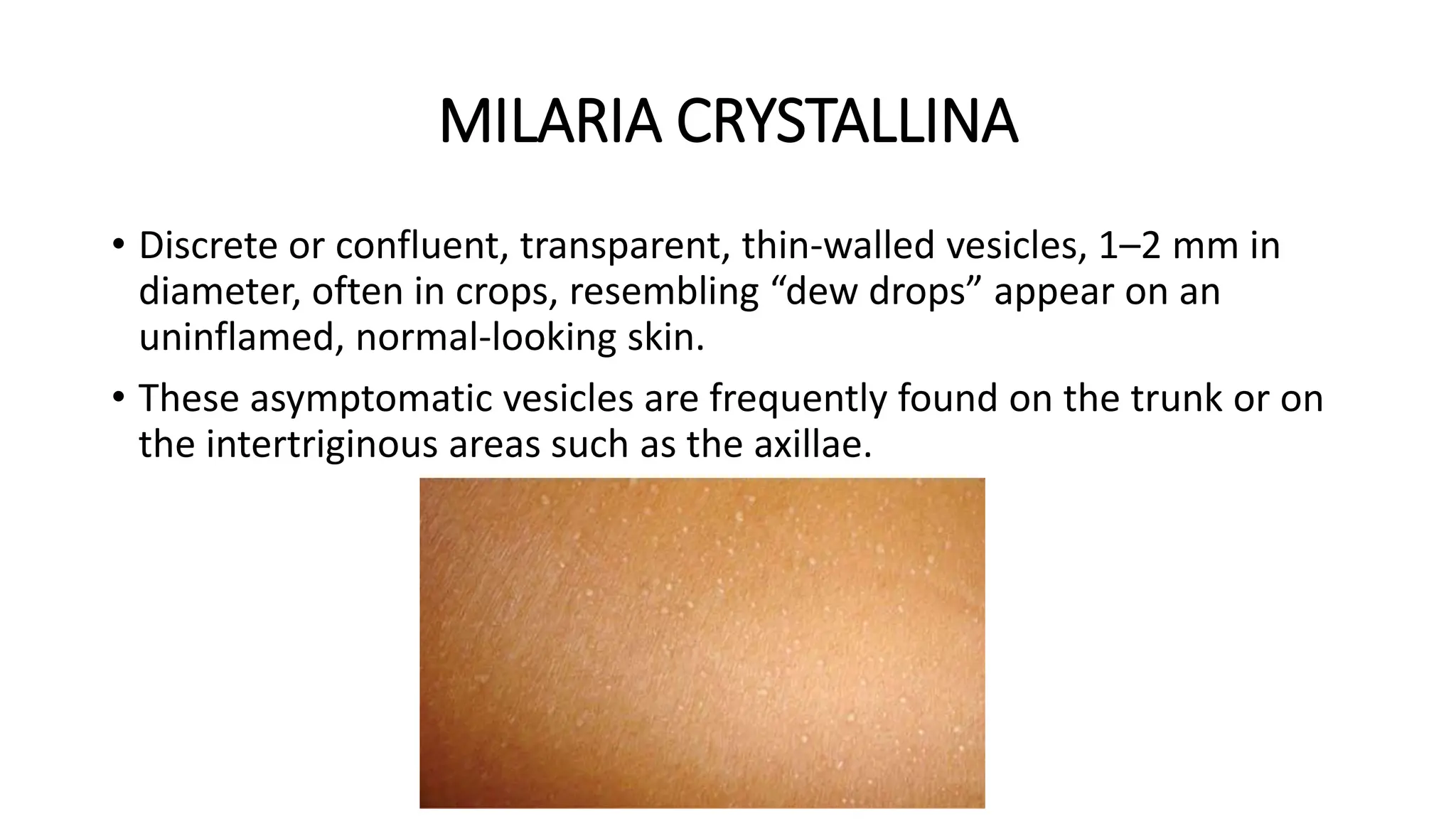
This document summarizes different types of sweat glands and disorders that can affect them. It discusses the three main types of sweat glands - eccrine, apocrine, and apoeccrine. The major disorder types covered are hyperhidrosis (excessive sweating) and hypohidrosis/anhidrosis (reduced or absent sweating). Treatment options are provided for different forms of hyperhidrosis that range from topical therapies to procedures like botulinum toxin injections or thoracic sympathectomy. Sweat retention syndromes like miliaria that cause skin eruptions are also summarized.