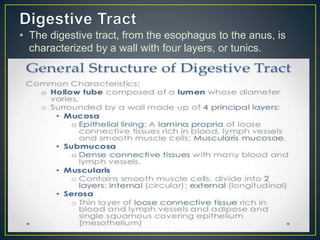
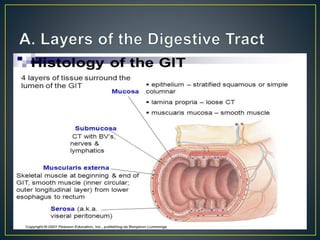
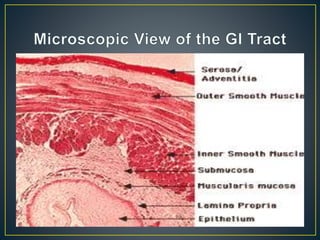
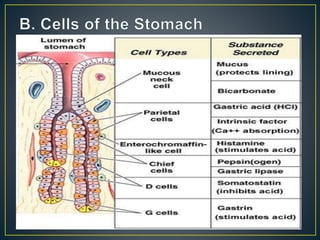
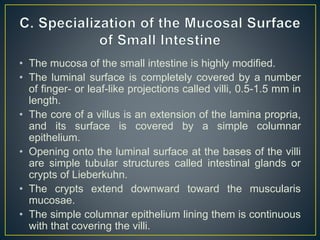
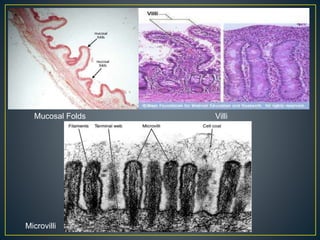
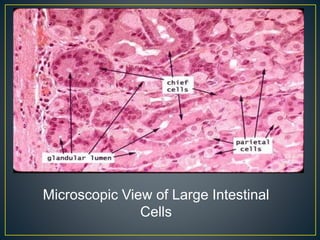
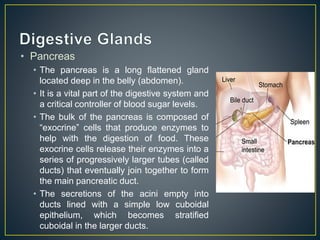
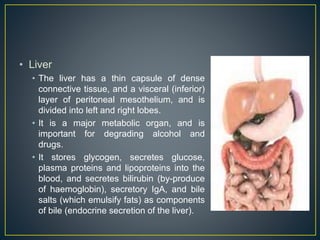
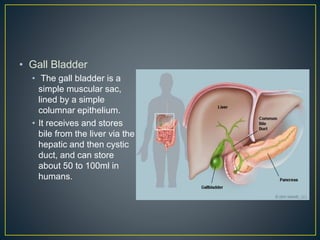
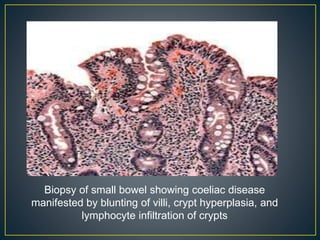
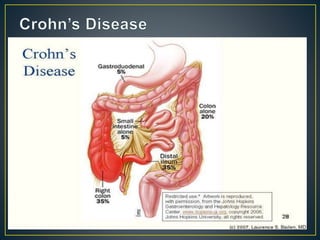
The document summarizes the major components and functions of the human digestive system. It describes the organs that make up the digestive tract, including the mouth, esophagus, stomach, small and large intestines, pancreas, liver, and gallbladder. It provides details on the layers of the digestive tract wall and specialized cells found in the stomach, small intestine, large intestine, pancreas, and liver that aid in digestion. The document also briefly discusses celiac disease, inflammatory bowel disease, and irritable bowel syndrome.