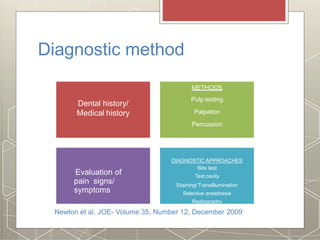
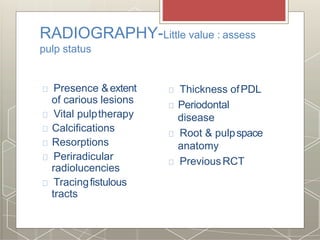
1) Diagnosis in endodontics involves gathering dental and medical history, performing clinical examinations and tests, and evaluating radiographs to determine the health, nature, and cause of issues with the pulp or surrounding tissues.
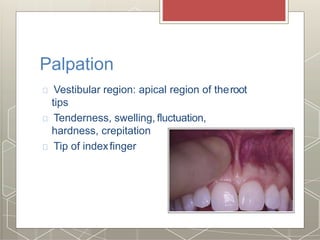
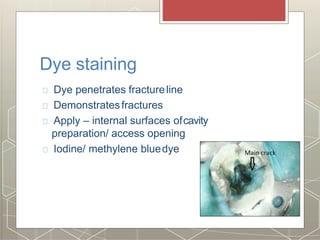
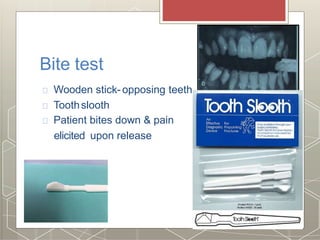
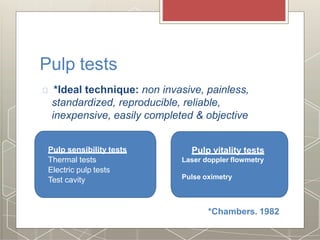
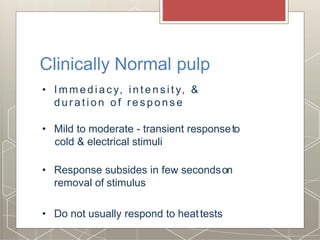
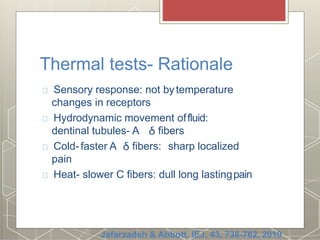
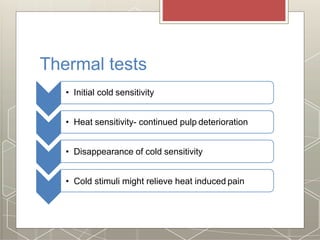
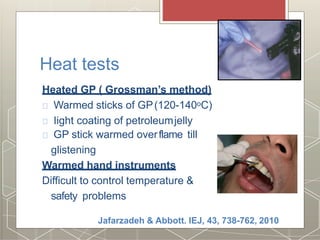
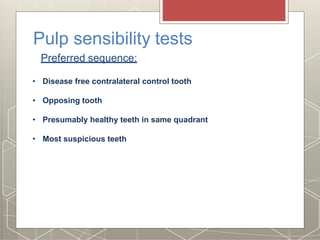
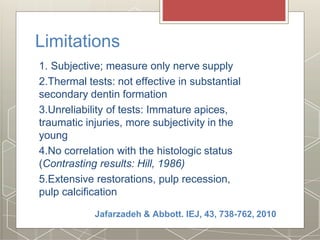
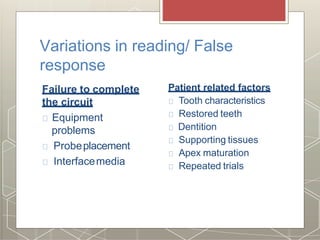
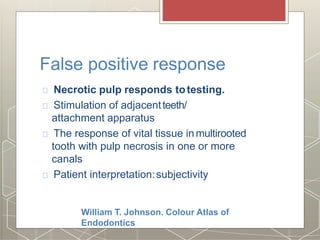
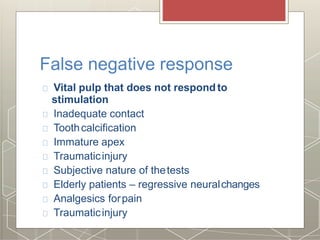
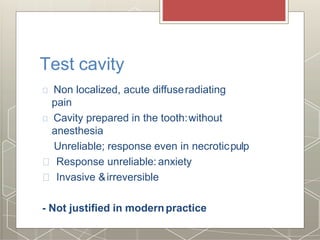
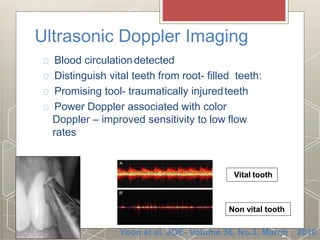
2) Clinical tests include thermal tests, electric pulp testing, percussion, palpation, and periodontal probing to evaluate the patient's response and assess pulp vitality or presence of pathology.
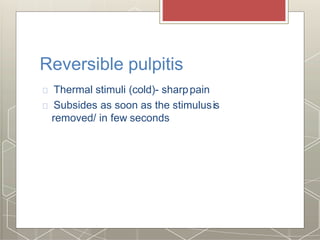
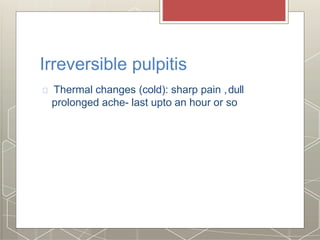
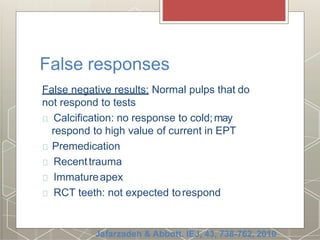
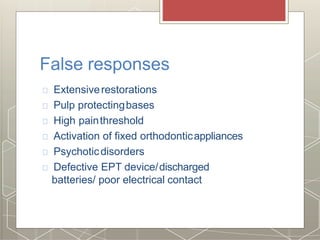
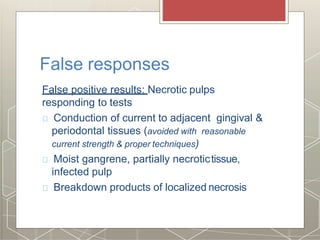
3) While no single test can definitively diagnose pulp status, cold tests are often more accurate than heat or electric pulp testing. Radiographs provide additional information but cannot solely determine a diagnosis.