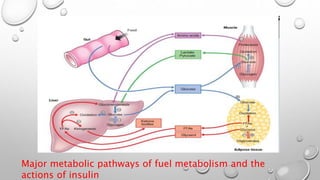
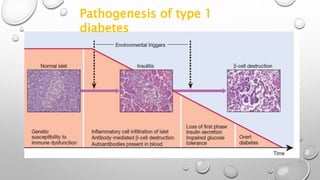
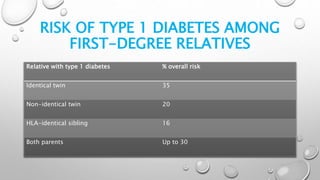
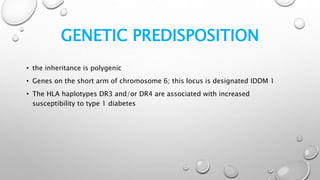
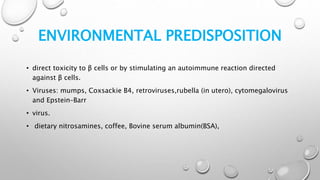
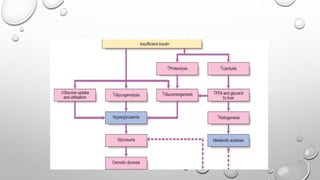
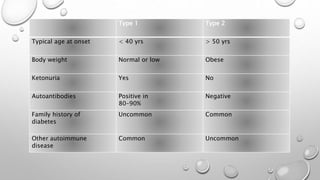
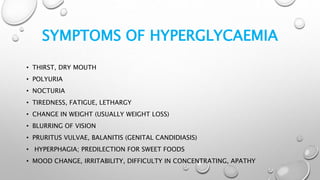
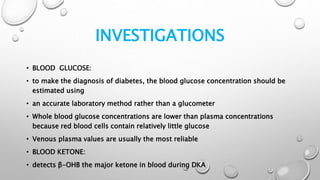
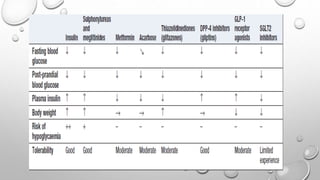
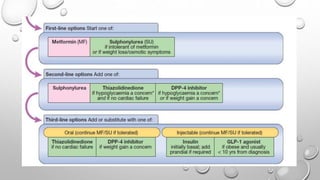
This document provides information on diabetes mellitus, including the main types of diabetes, their causes, clinical features, diagnosis, and treatment. It discusses type 1 and type 2 diabetes in detail. Type 1 diabetes is an autoimmune disease resulting in destruction of insulin-producing beta cells, while type 2 diabetes involves insulin resistance and relative insulin deficiency. Diagnosis involves blood glucose and HbA1c testing. Treatment includes lifestyle changes, oral medications like metformin and sulfonylureas, and insulin for managing blood glucose levels. The goal of treatment is to control blood glucose and reduce risk of complications.