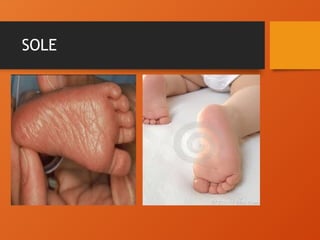
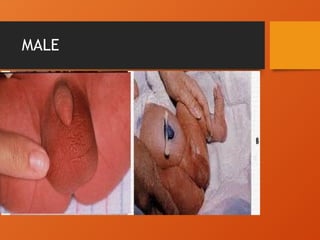
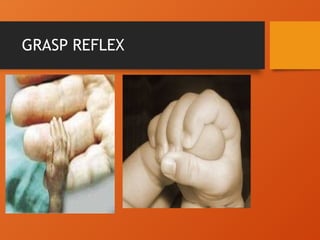
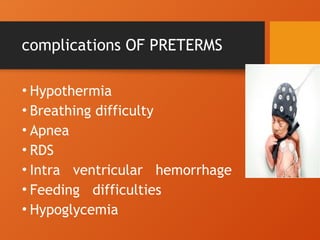
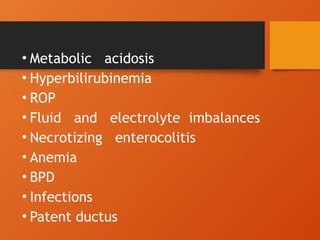
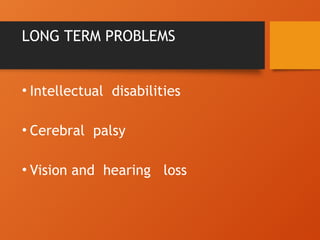
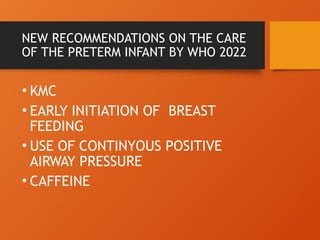
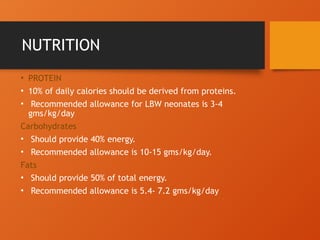
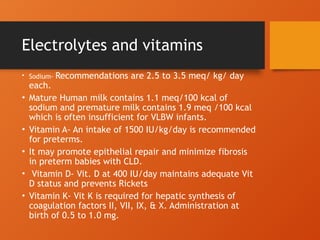
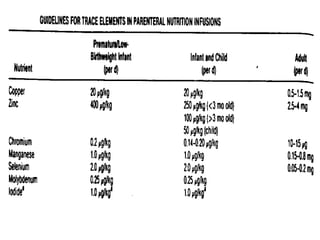
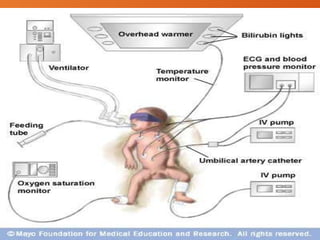
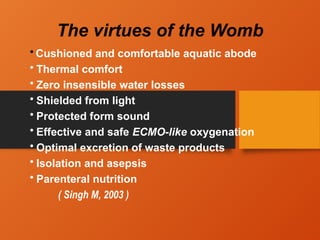
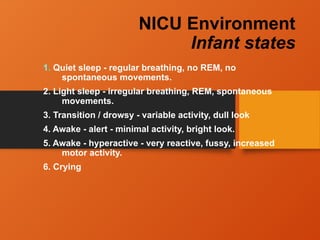
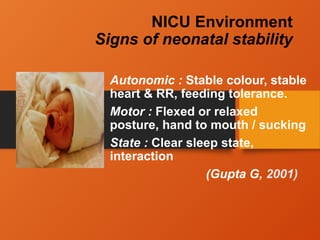
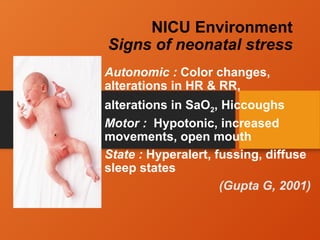
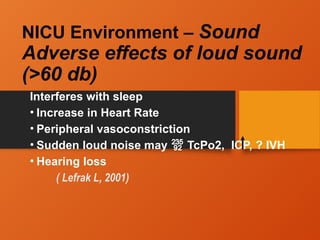
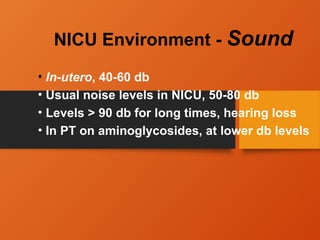
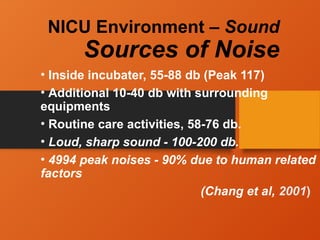
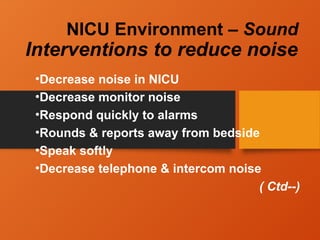
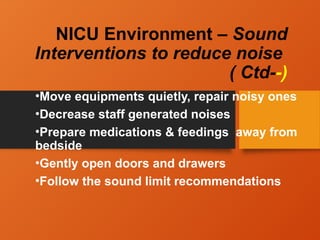
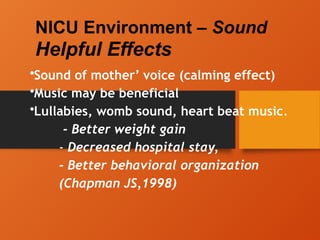
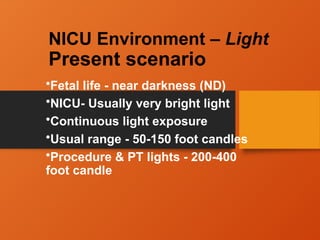
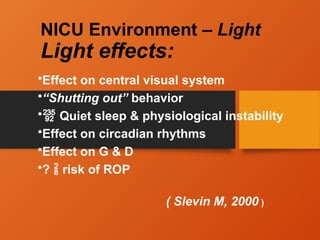
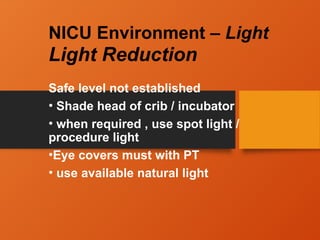
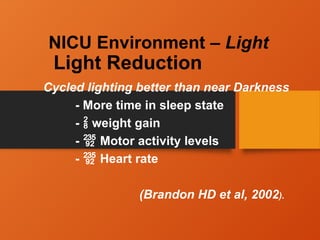
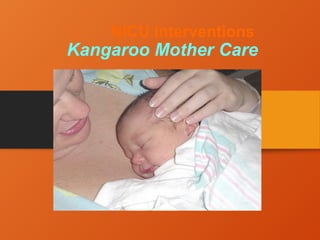
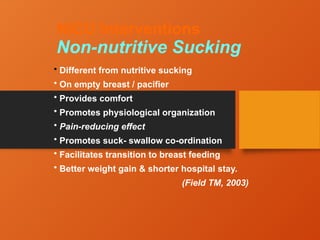
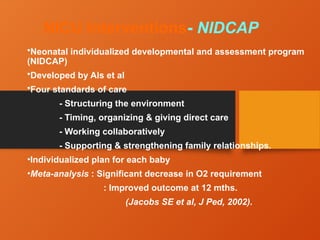
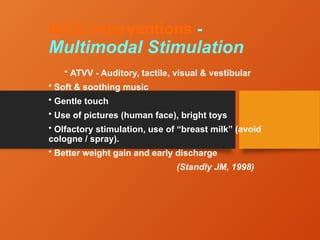
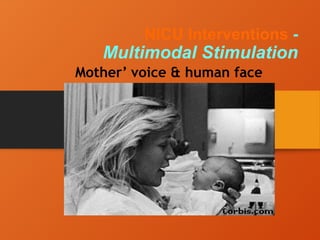
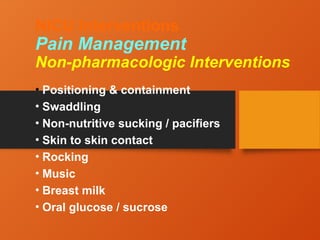
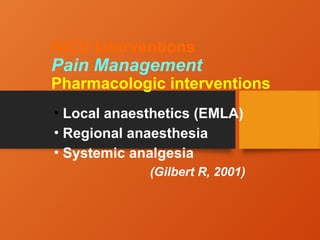
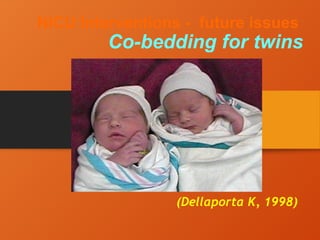
The document discusses the care and management of preterm infants, detailing their classifications, characteristics, and common complications. It highlights new WHO recommendations for their care, including nutritional guidelines and interventions such as kangaroo mother care and developmental support strategies. Additionally, it emphasizes the importance of the NICU environment, addressing sound and light levels, positioning, and family involvement in care.