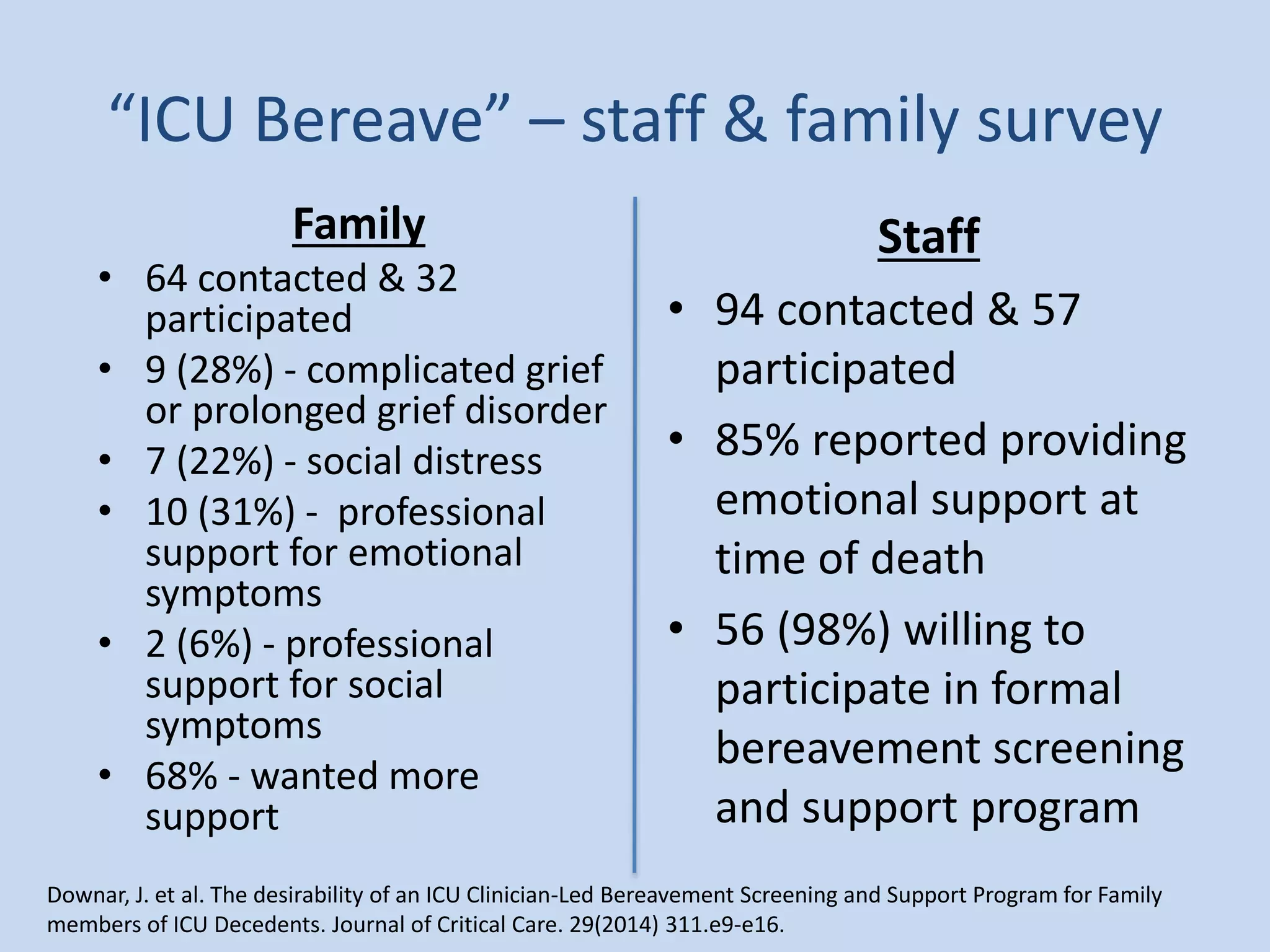
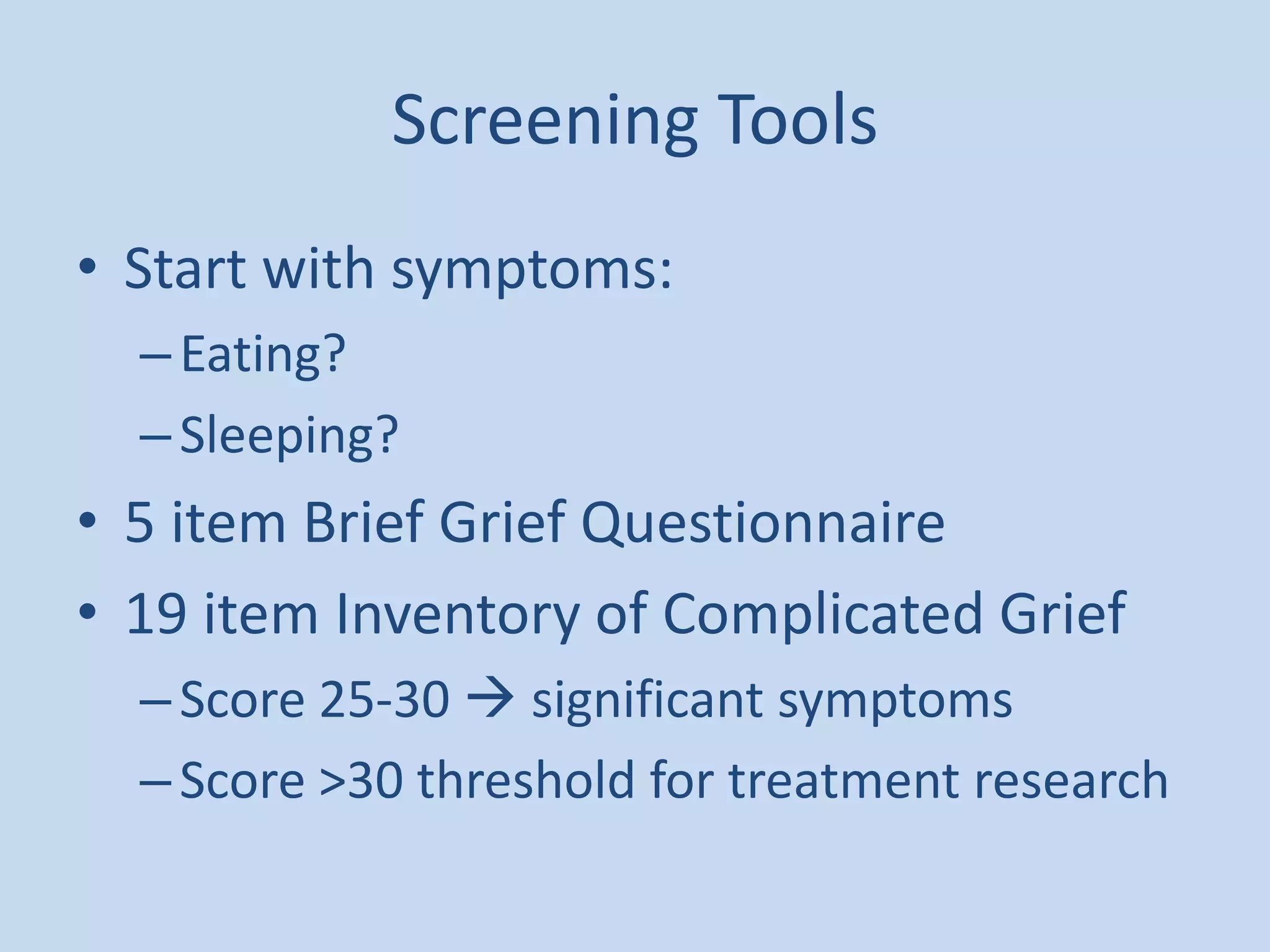
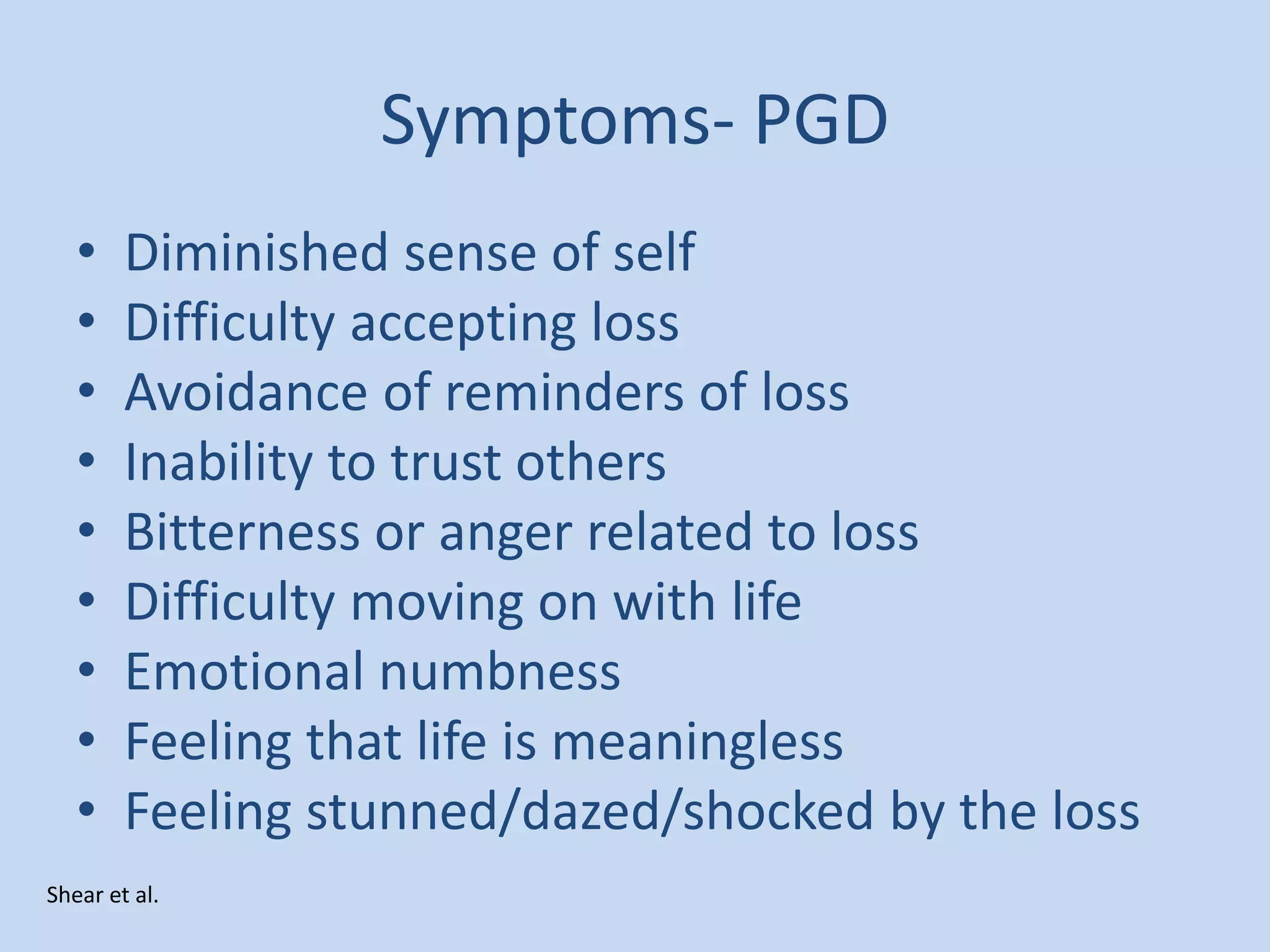
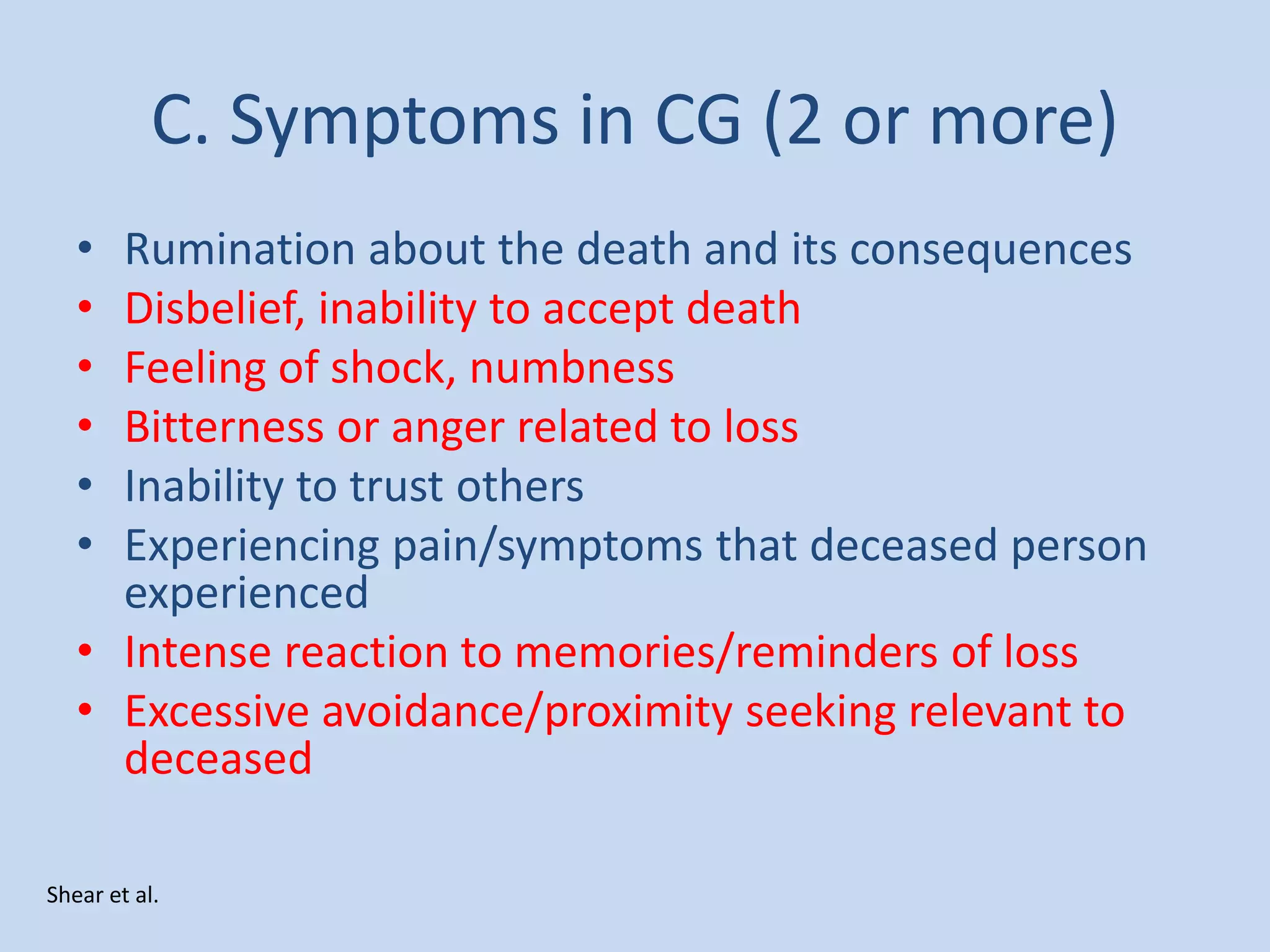
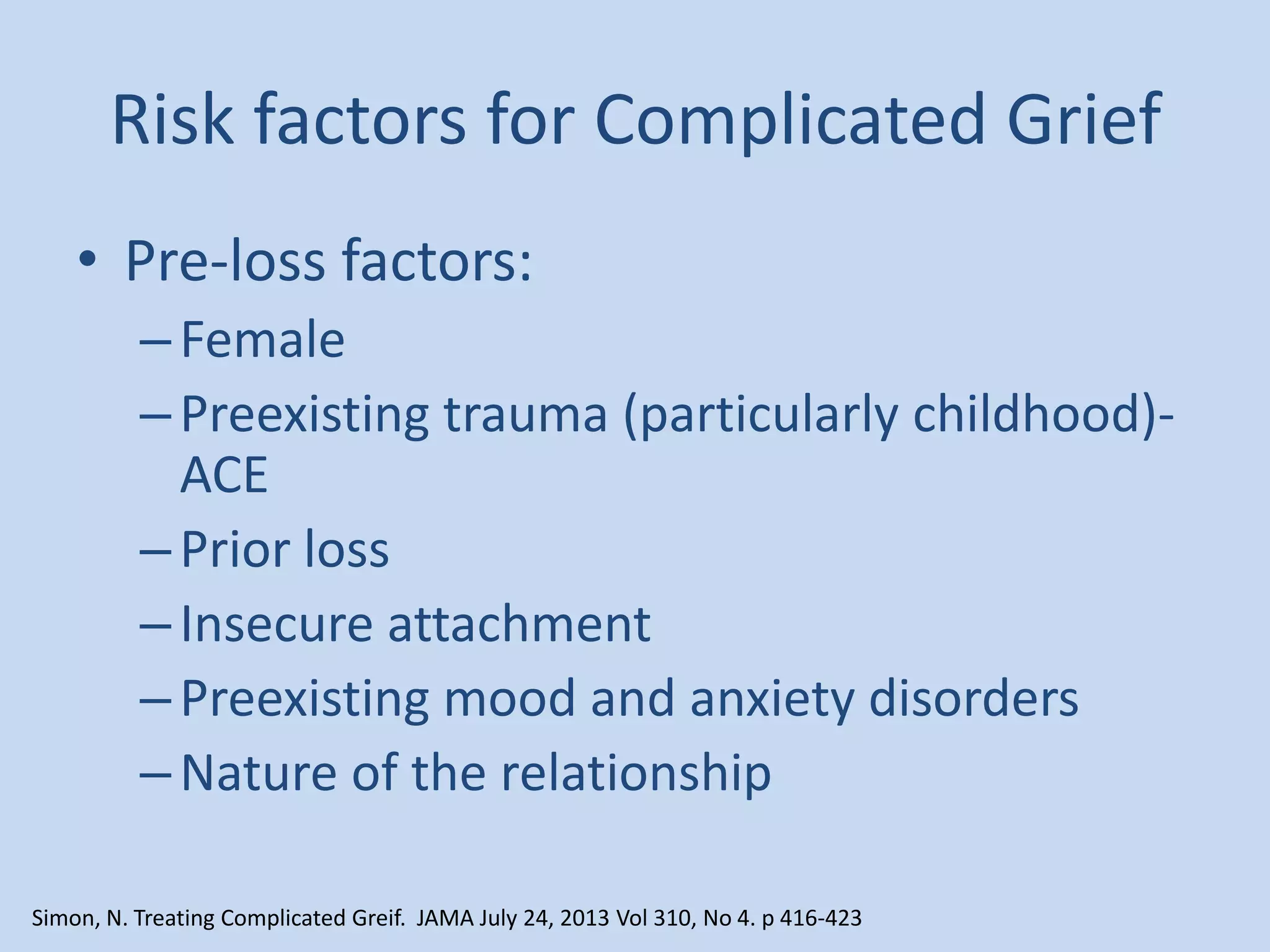
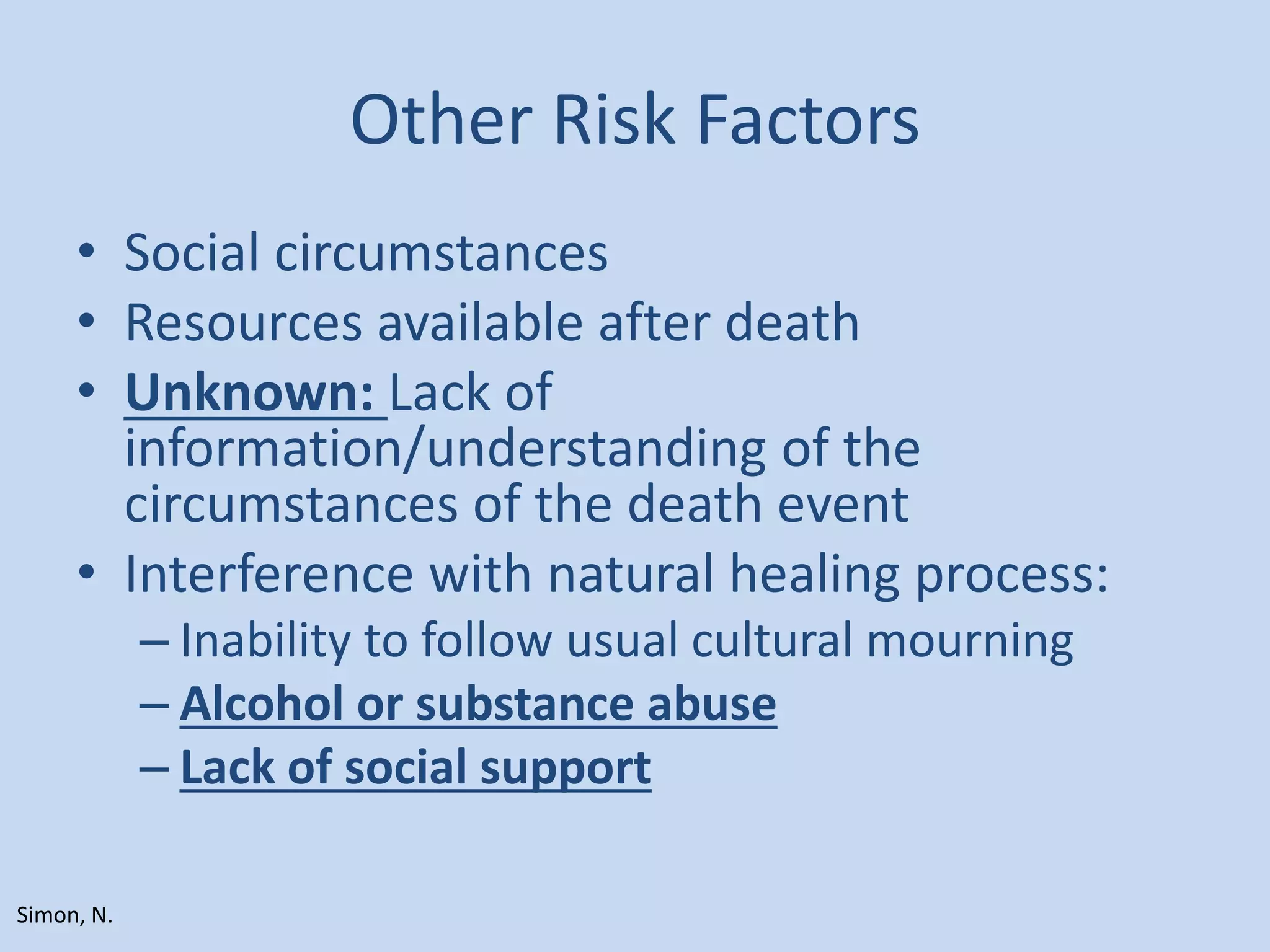
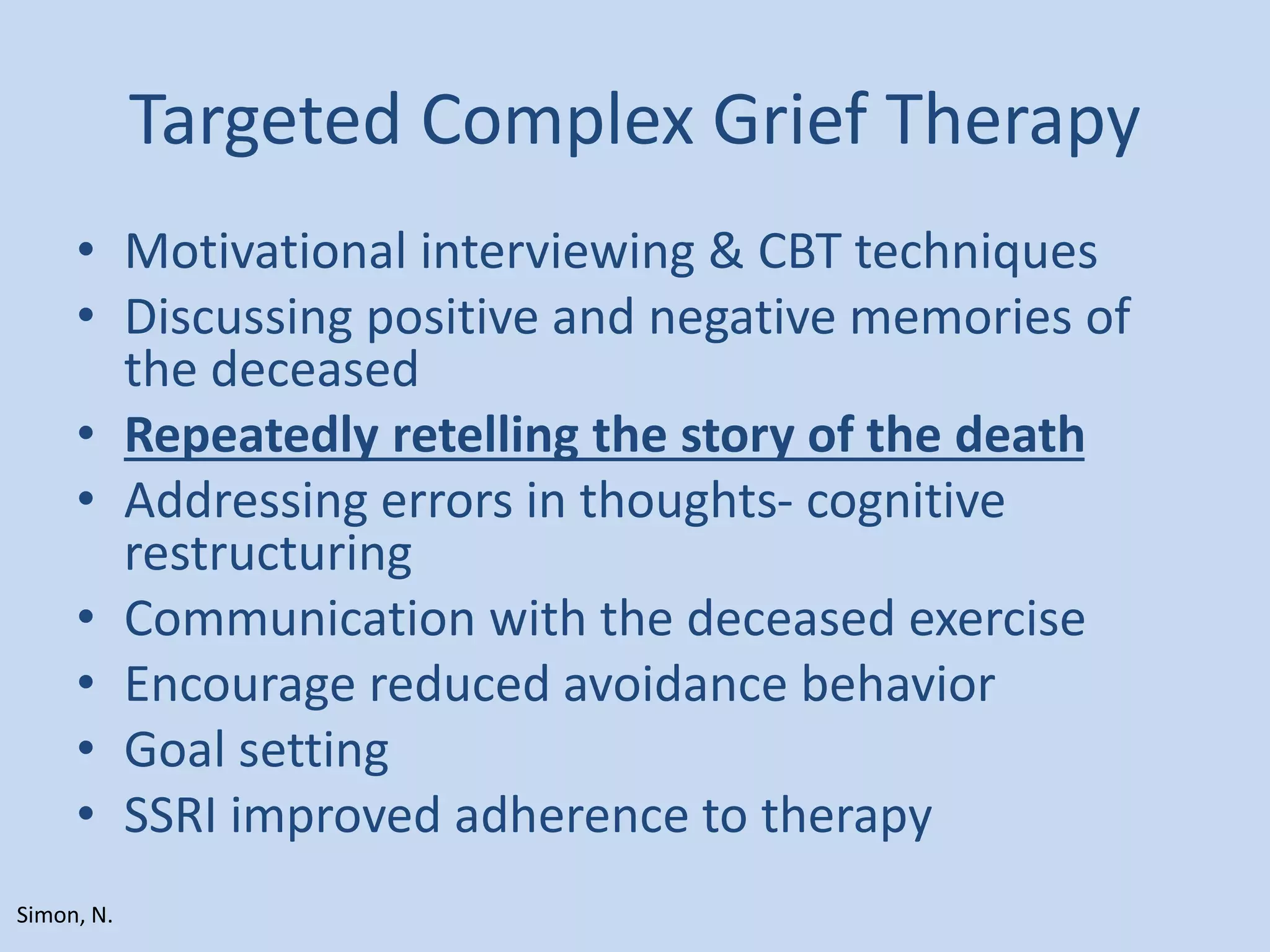
This document summarizes a presentation on end of life grief and bereavement. It discusses grief theories, typical and complicated grief, screening tools for complicated grief, and interventions. It also covers special considerations for bereavement in populations like those who experience perinatal loss or losing a child. Risk factors for complicated grief are identified and treatments like cognitive behavioral therapy and medications are outlined.