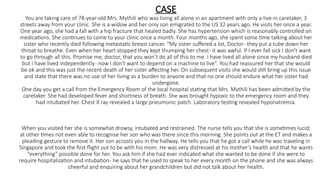
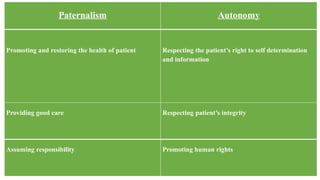
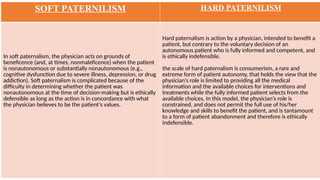
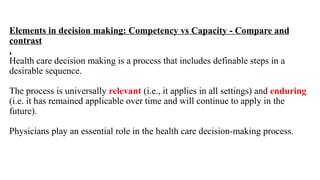
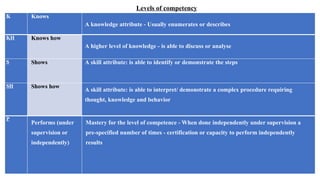
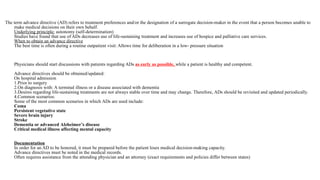
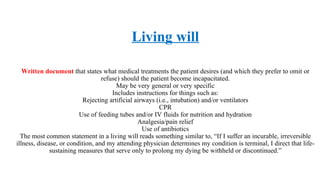
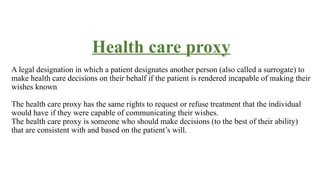
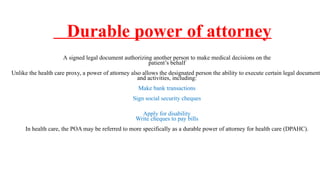
The document discusses bioethics related to patient autonomy, decision-making, and advance directives through the case study of Mrs. Mythili, an elderly patient with specific wishes regarding life-sustaining treatment. It outlines the principles of autonomy and beneficence, the significance of competence and capacity in medical decision-making, and details various types of advance directives, including living wills and health care proxies. Additionally, it addresses the complexities of paternalism and the ethical implications of respecting patient wishes against family directives in critical care scenarios.