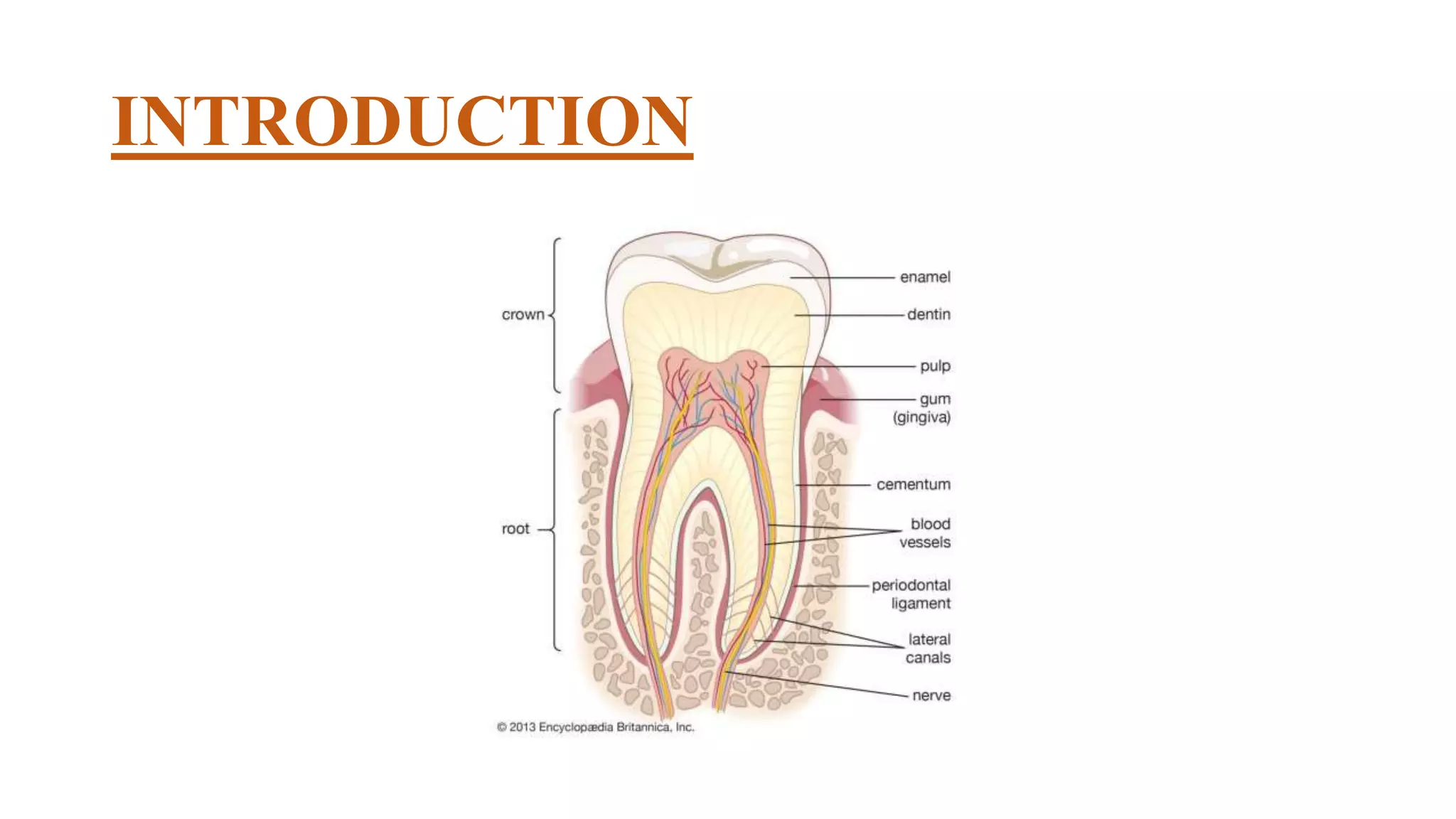
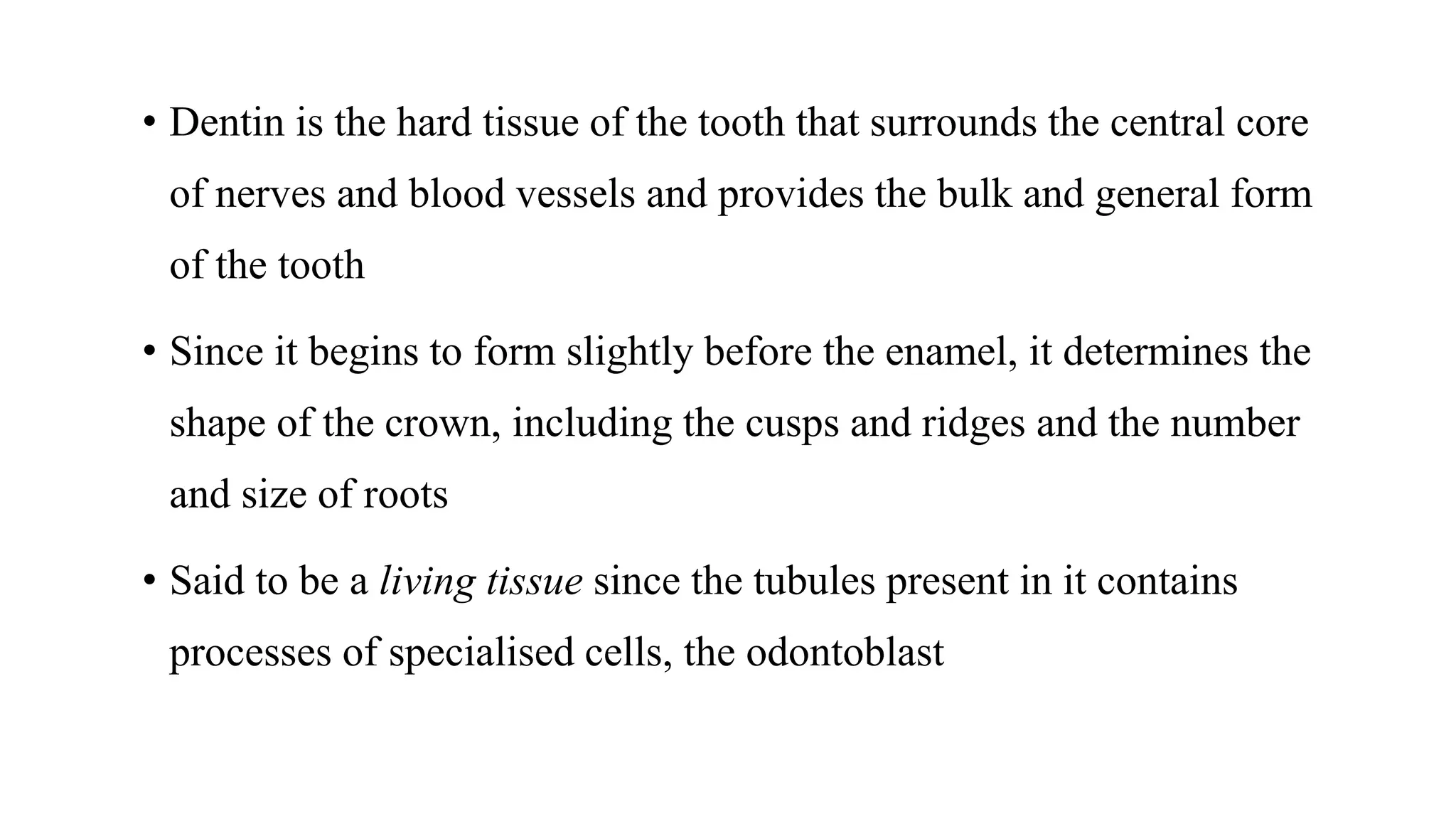
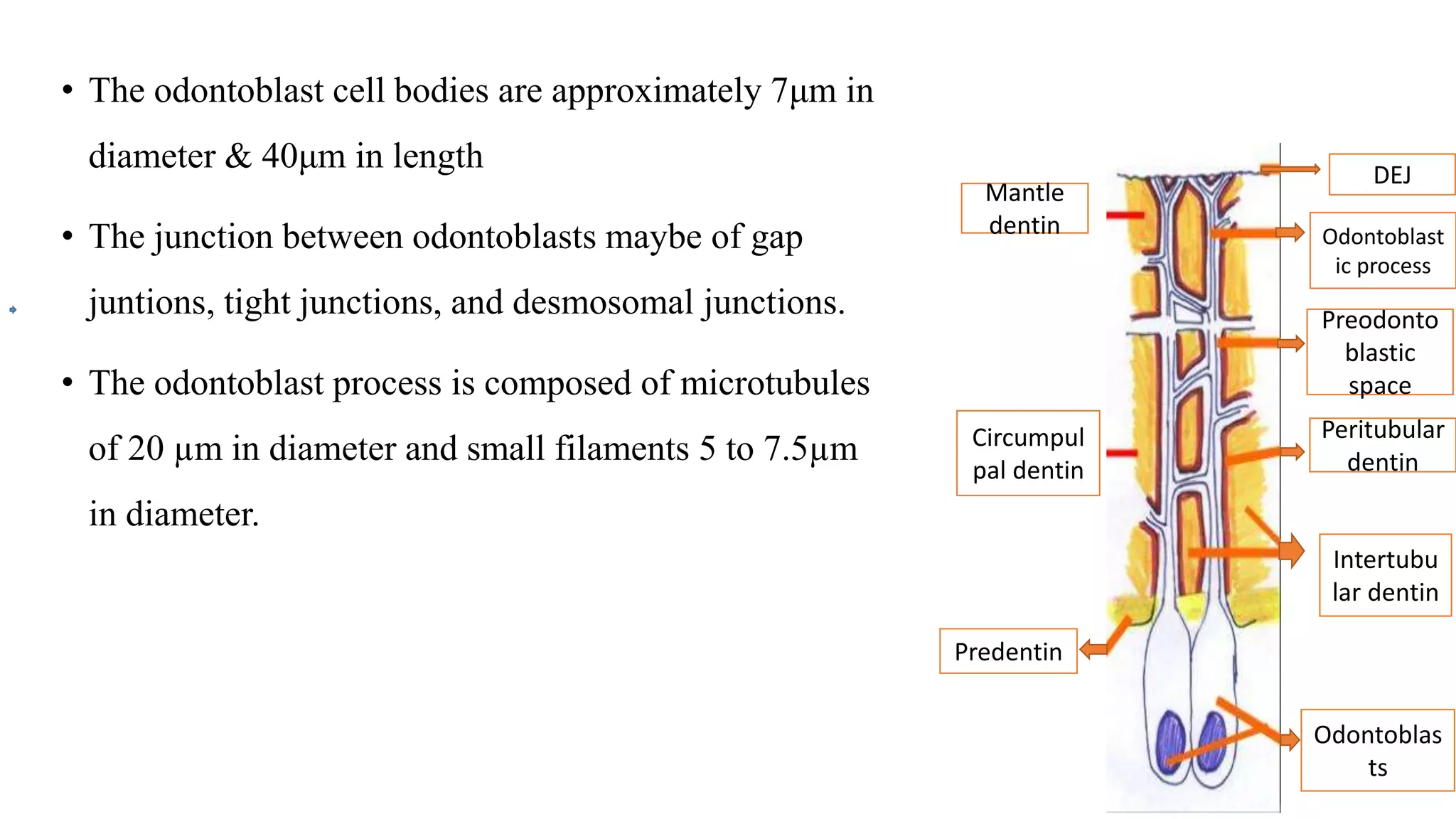
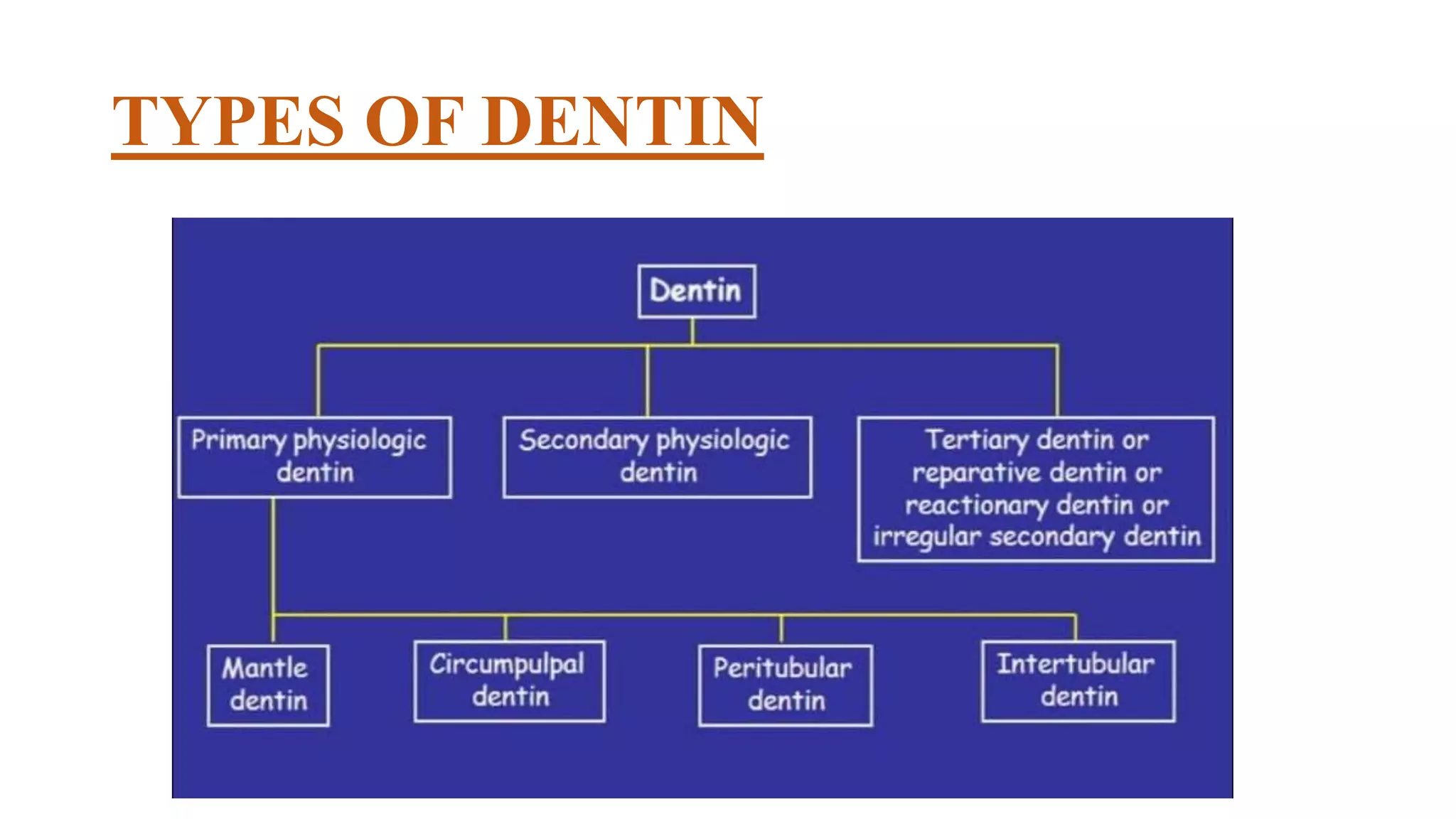
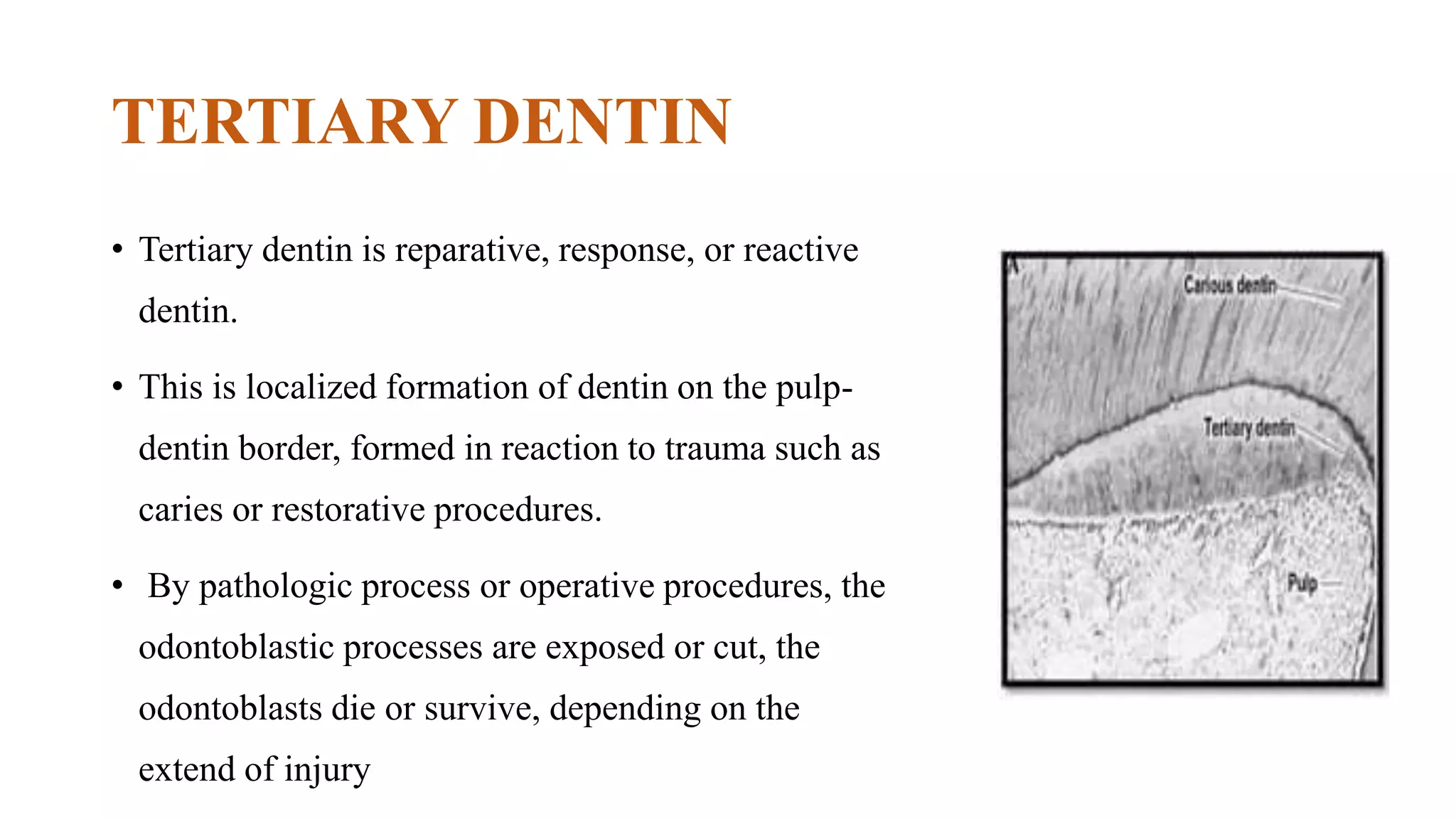
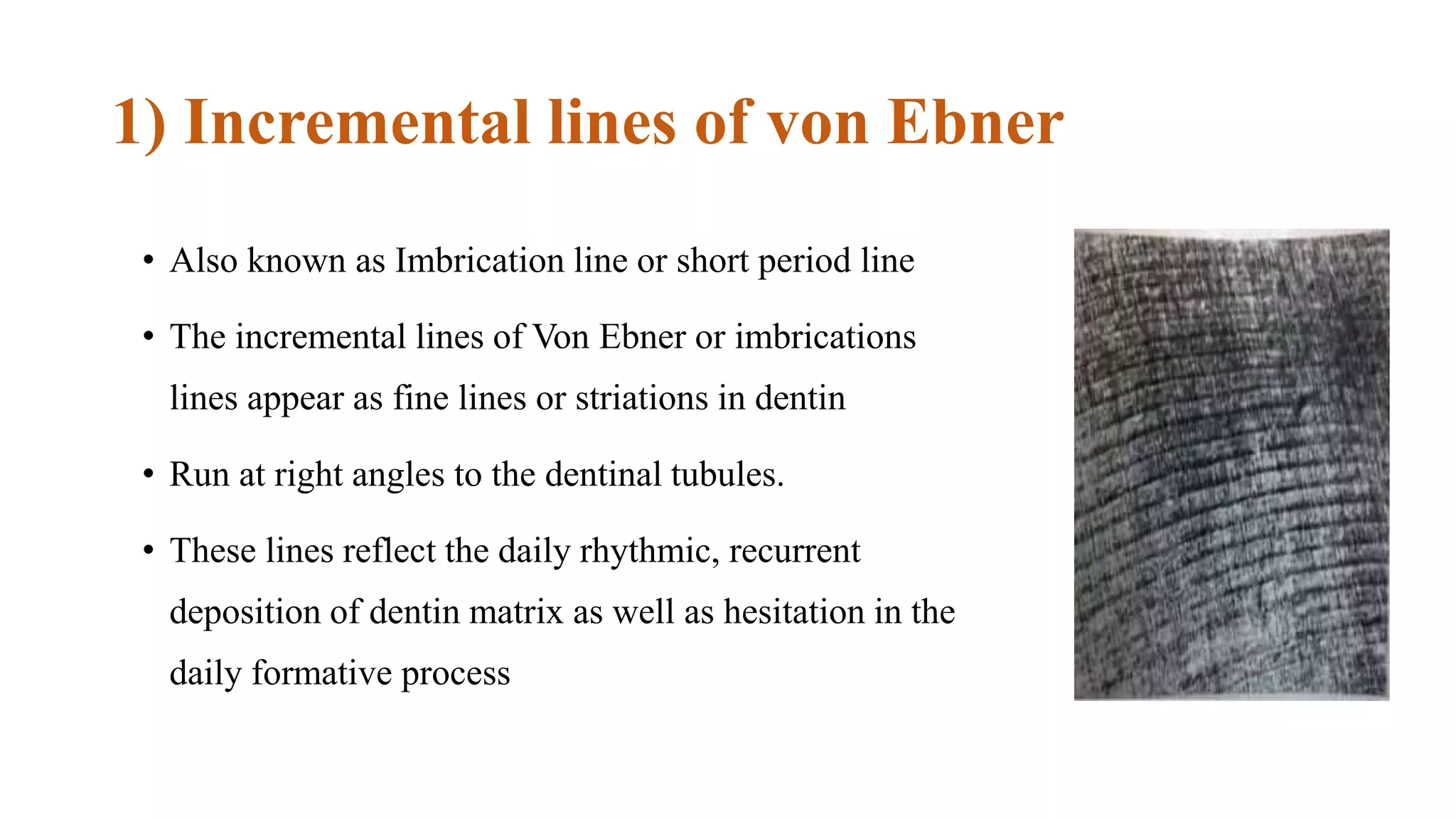
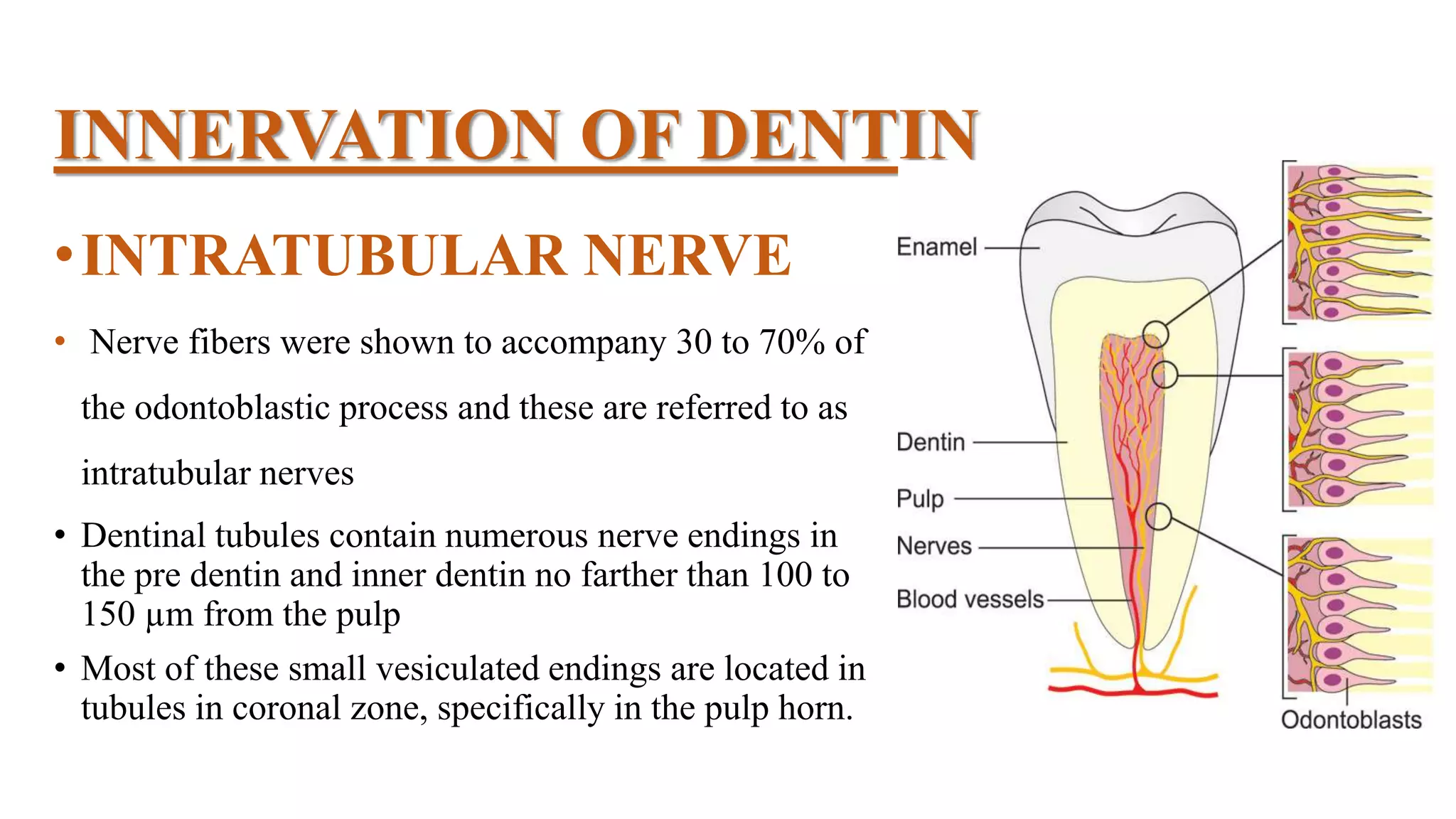
This document provides an overview of dentin, including its physical, chemical, and structural properties. It discusses the types of dentin such as primary, secondary, and tertiary dentin. It describes the development of dentin through odontoblast differentiation and matrix formation followed by mineralization. Key structures of dentin like dentinal tubules, peritubular dentin, and predentin are defined. Theories of pain transmission through dentin and age-related functional changes in dentin are also summarized.