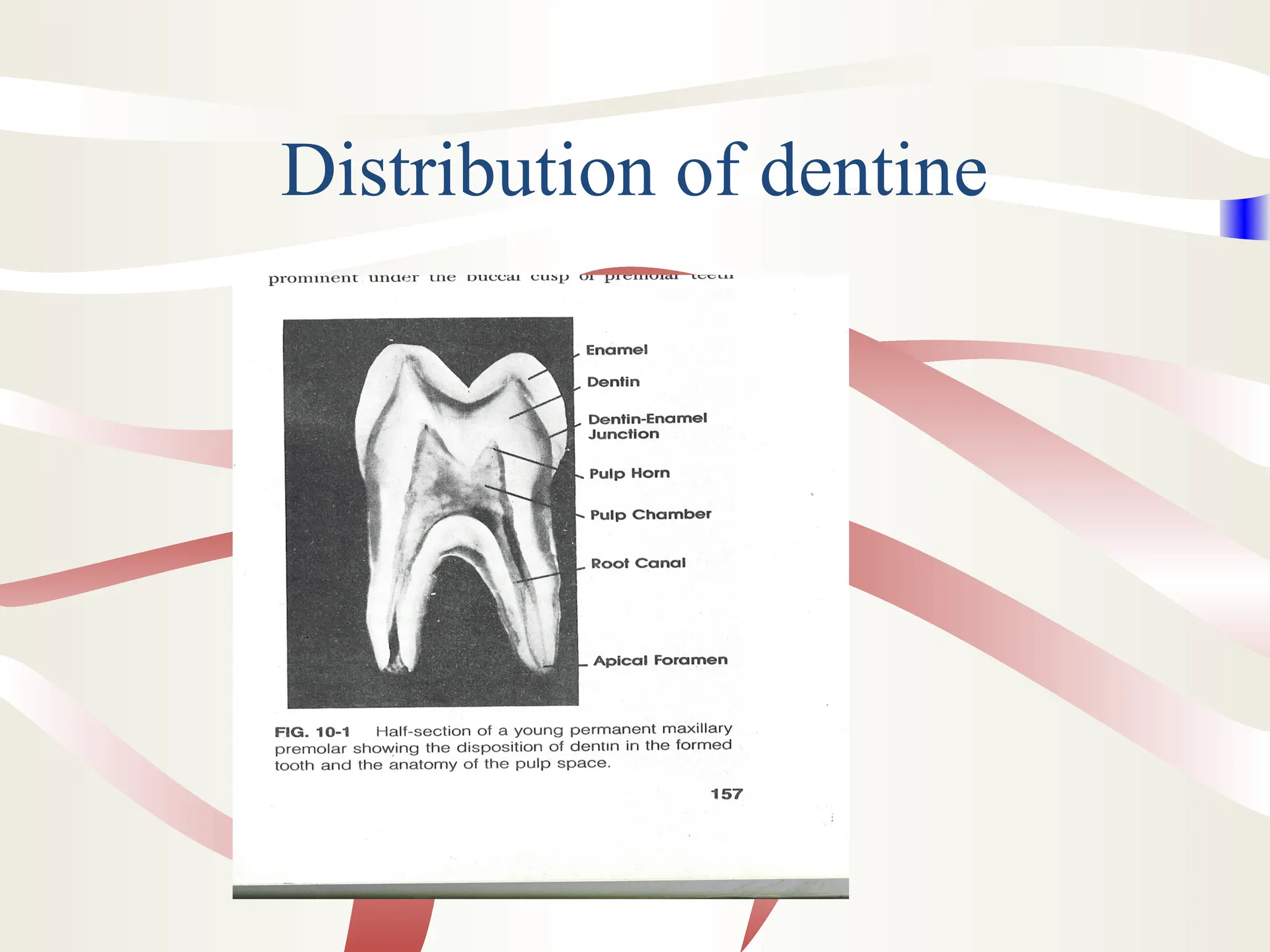
The document outlines the composition, structure, and types of dentine, covering aspects such as its physical and chemical properties, the formation and types of dentin (primary, secondary, and tertiary), and the mechanisms of dentine sensitivity. It explains the roles of odontoblasts in dentine formation, the importance of dentinal tubules, and various features like interglobular dentine and dead tracts. Additionally, the document discusses the process of dentinogenesis and the relationship of dentine to other dental tissues.