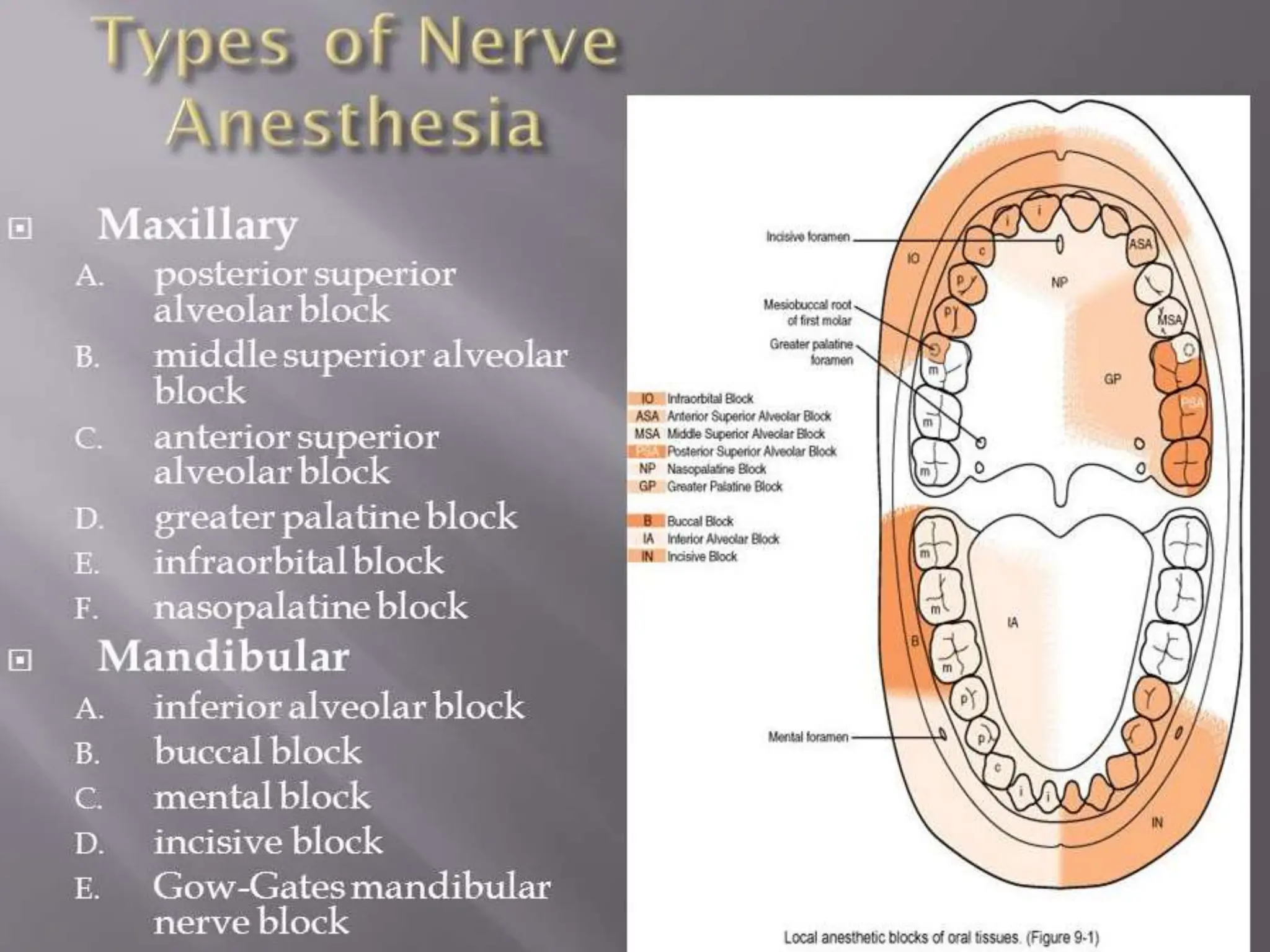
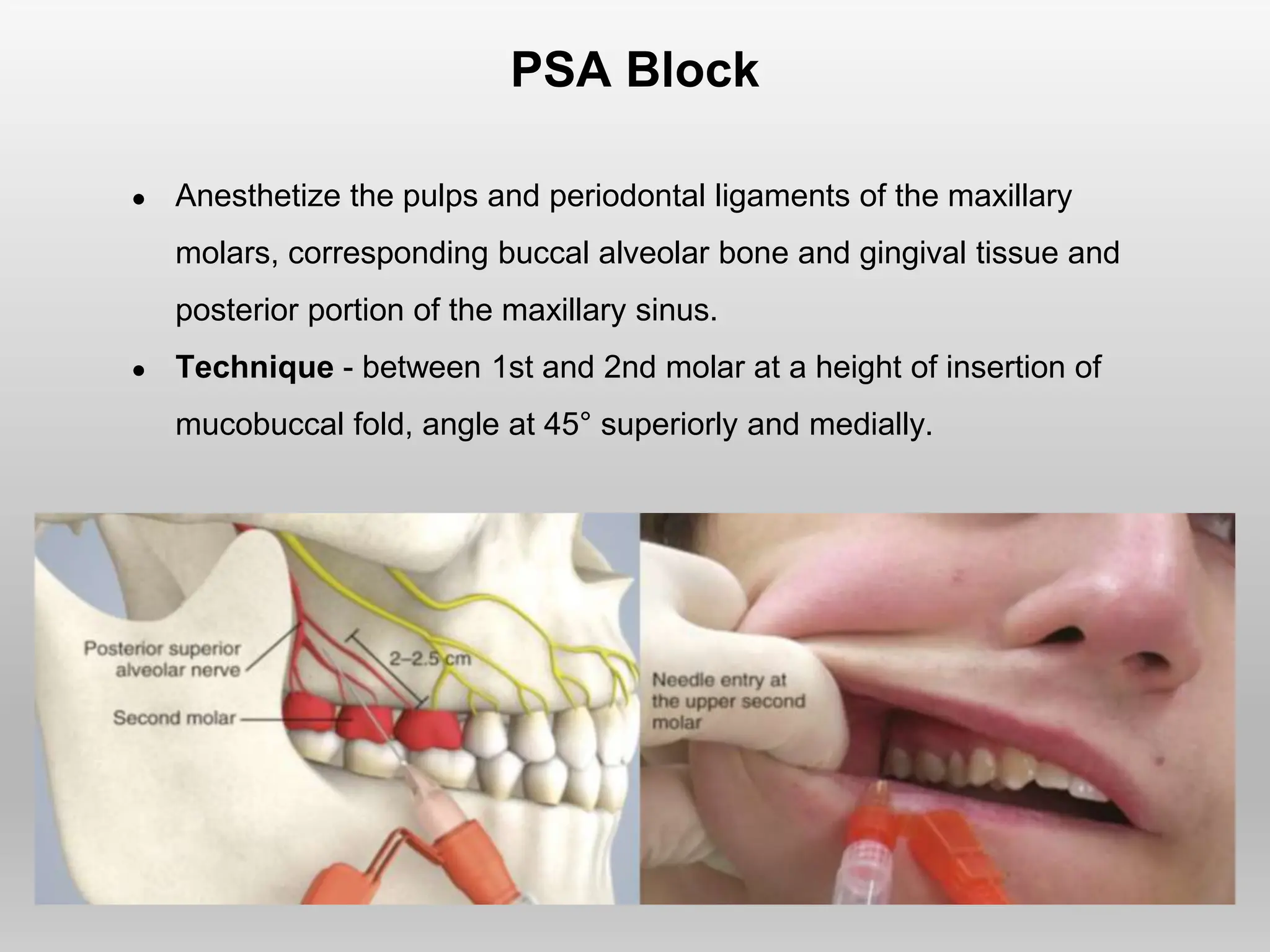
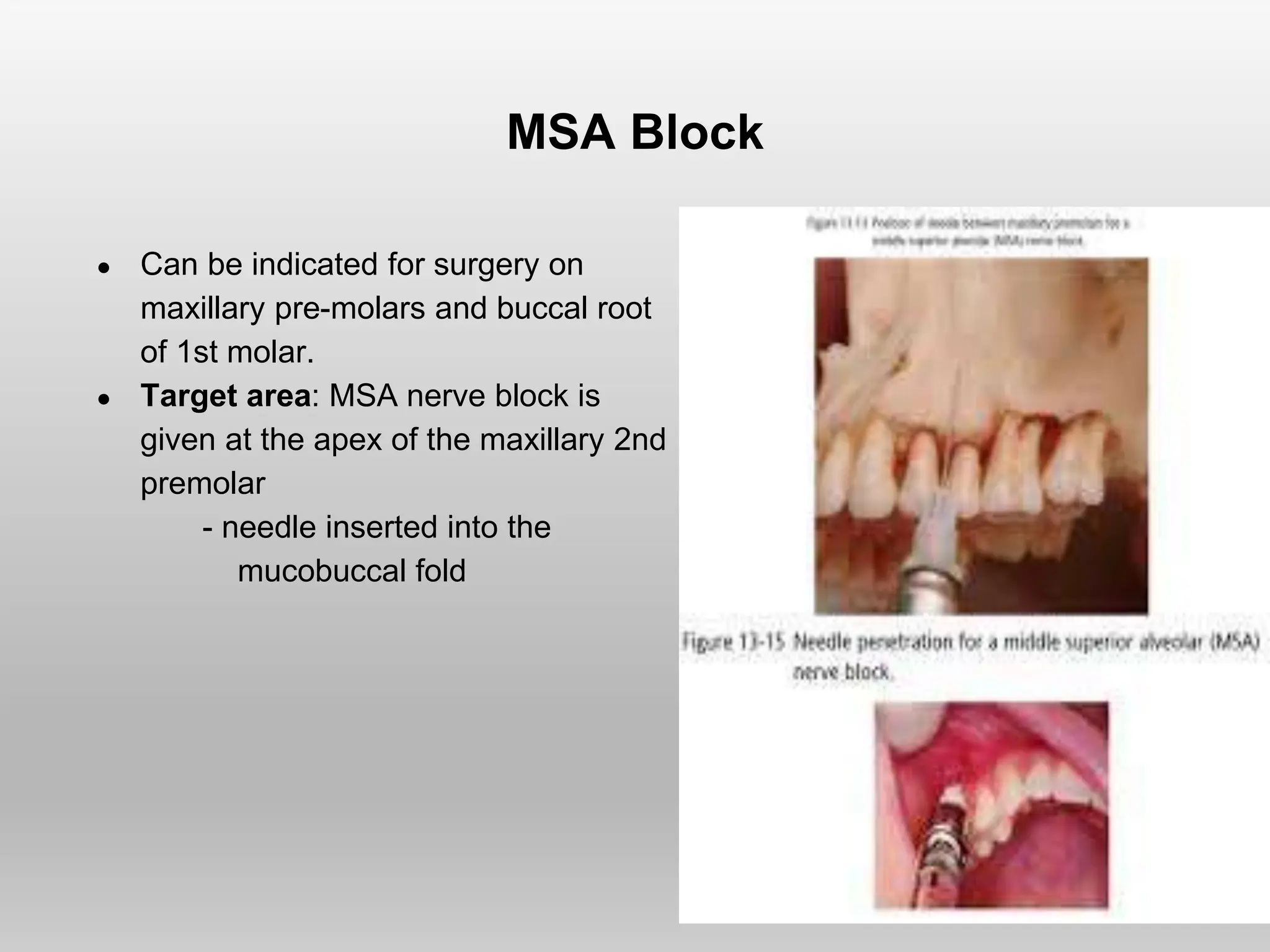
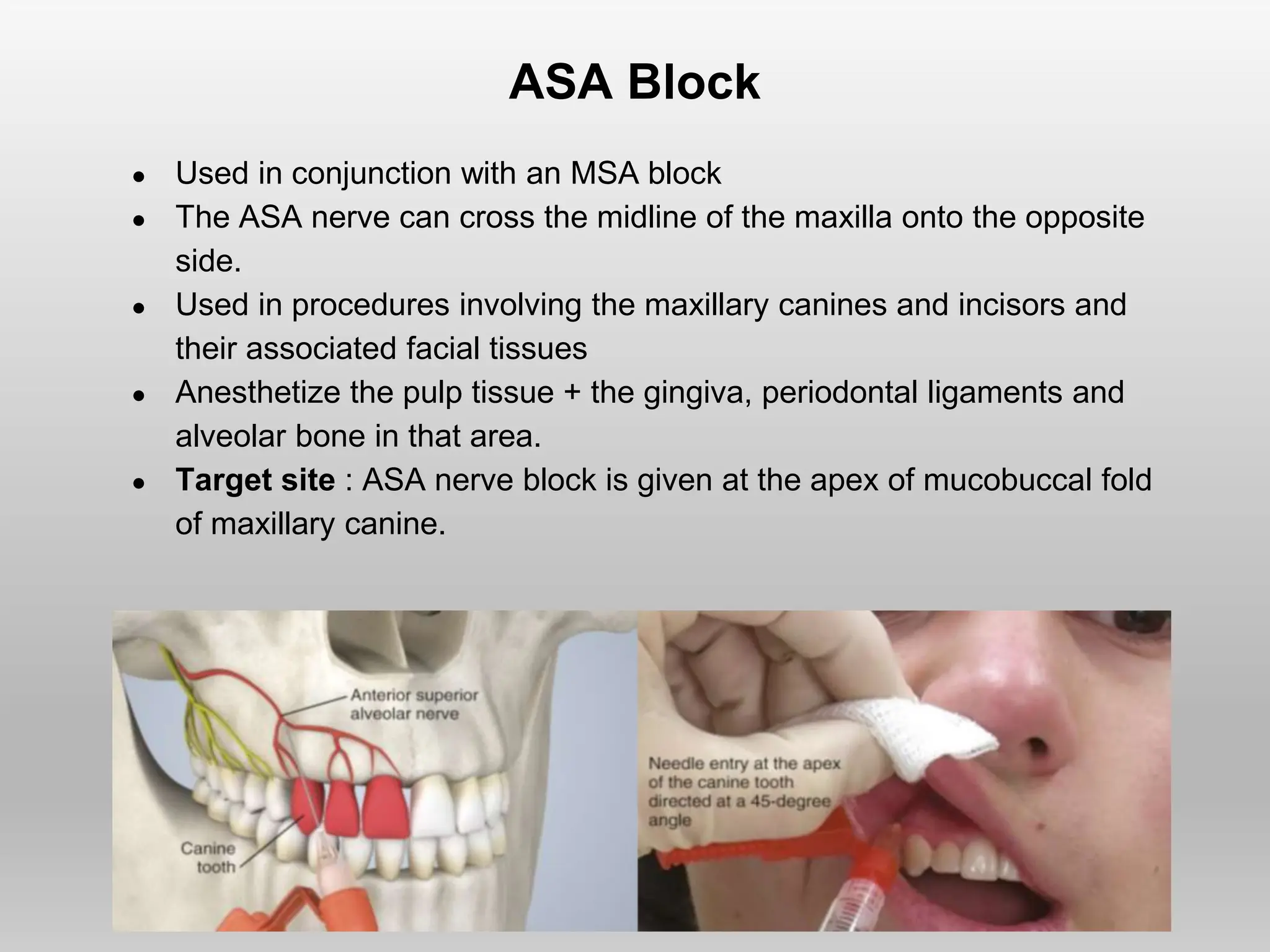
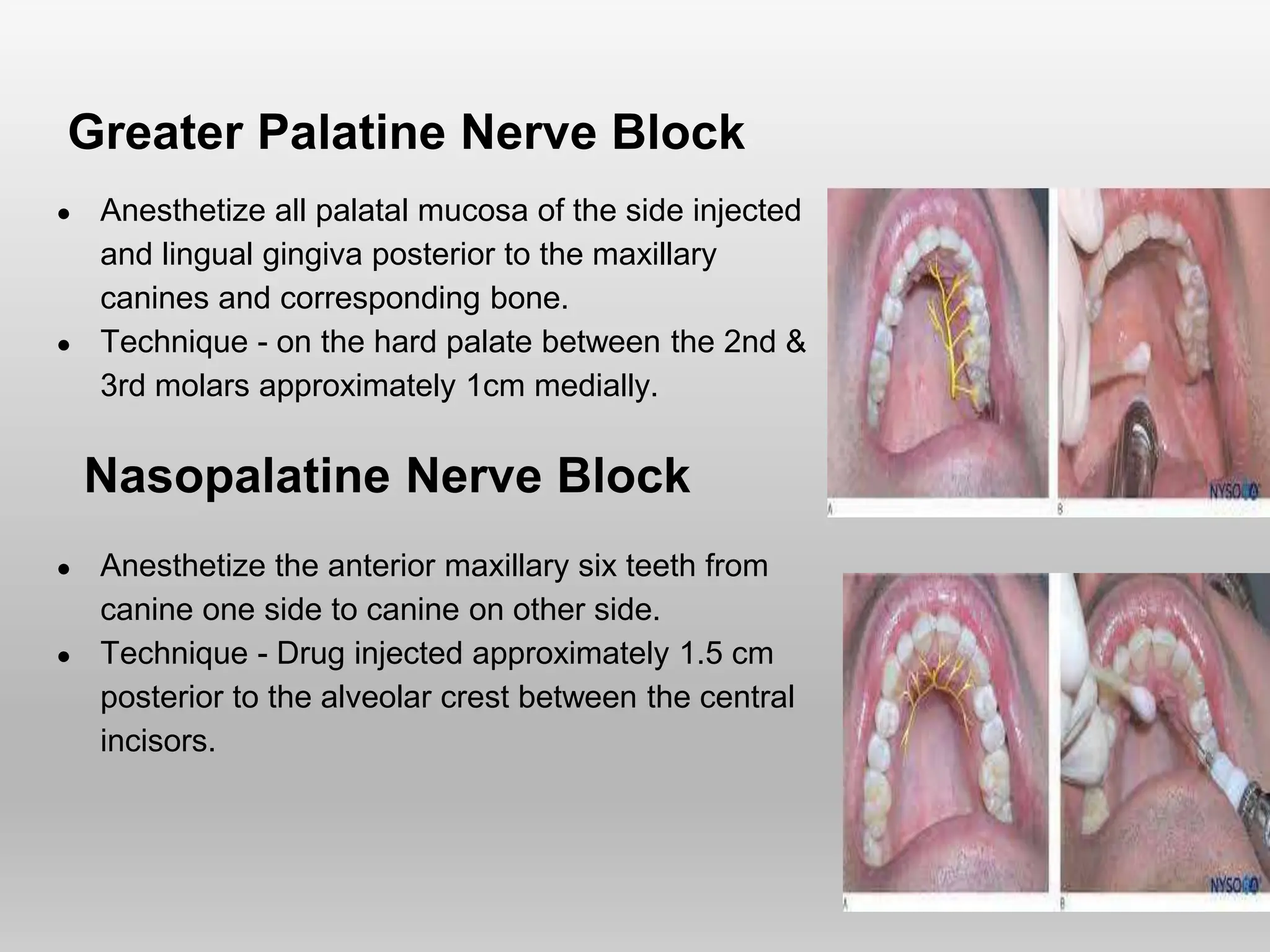
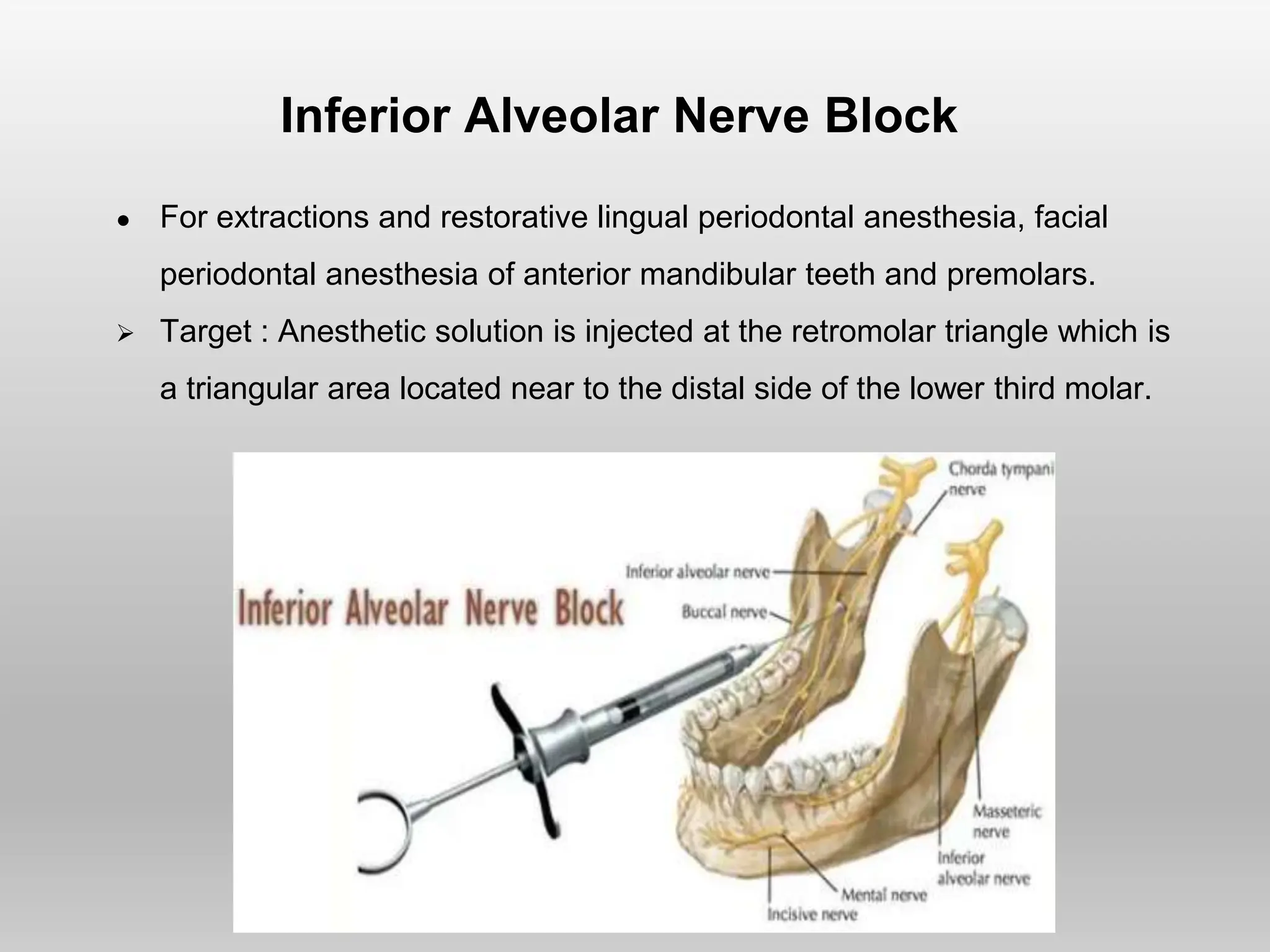
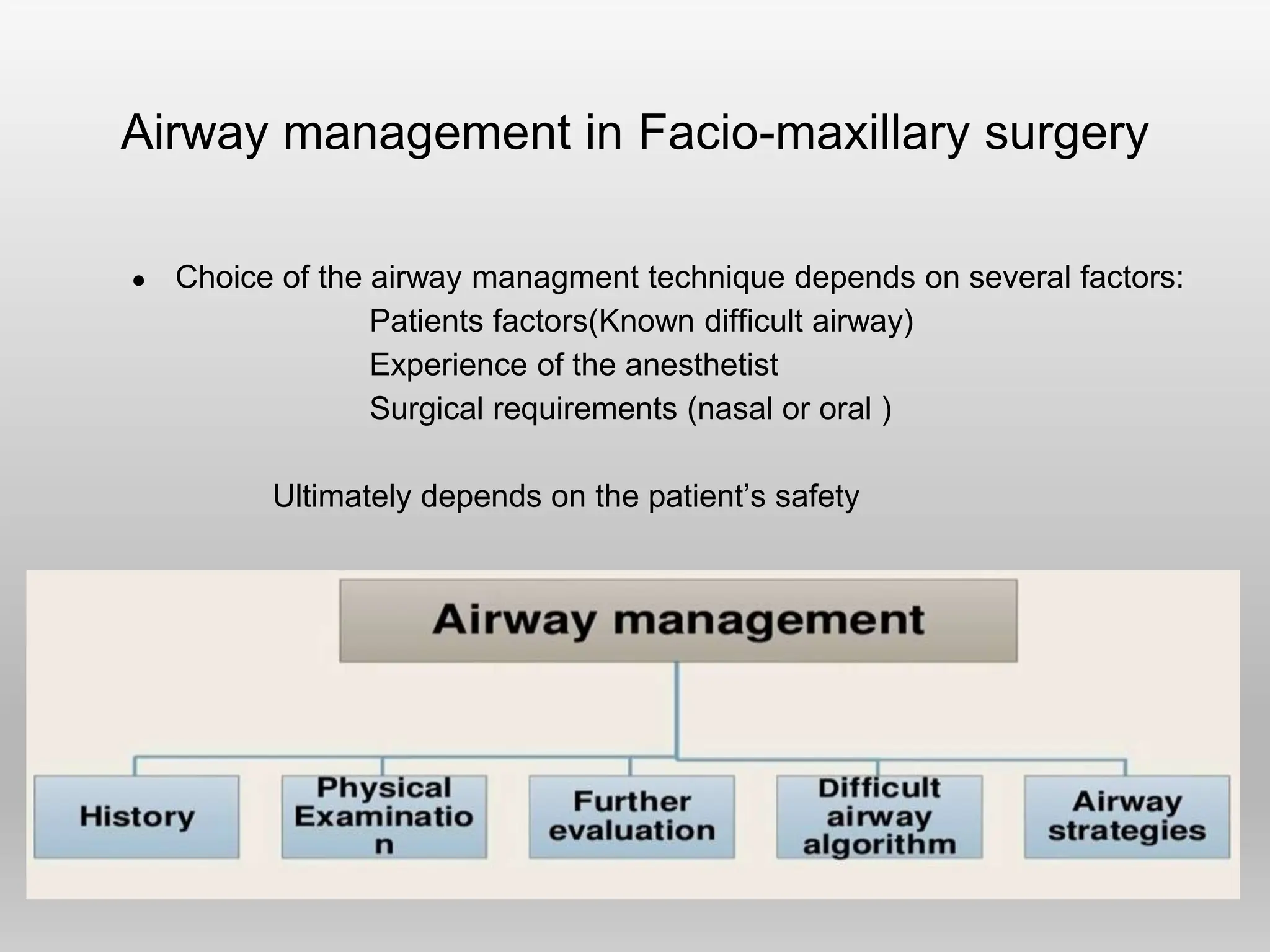
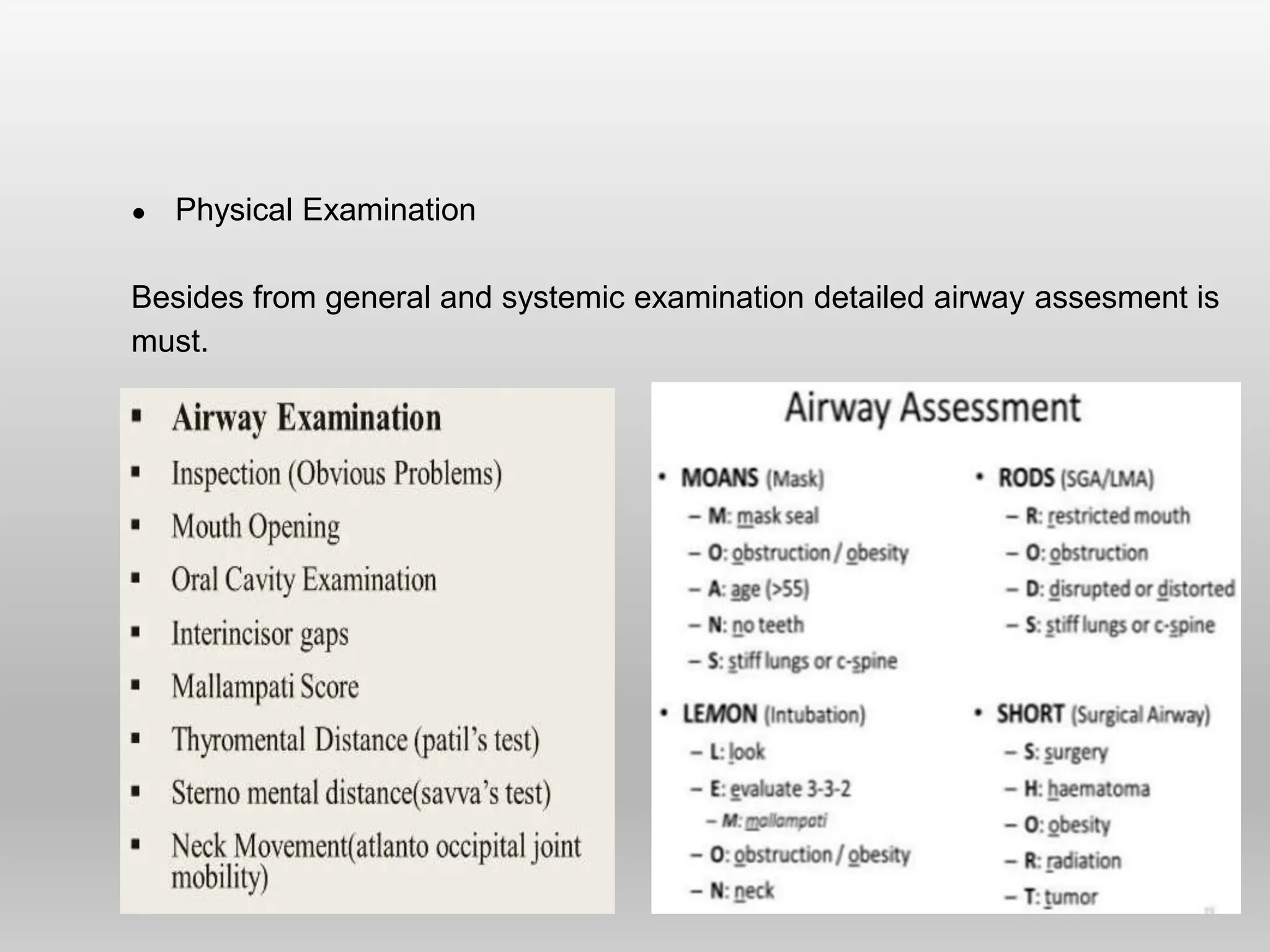
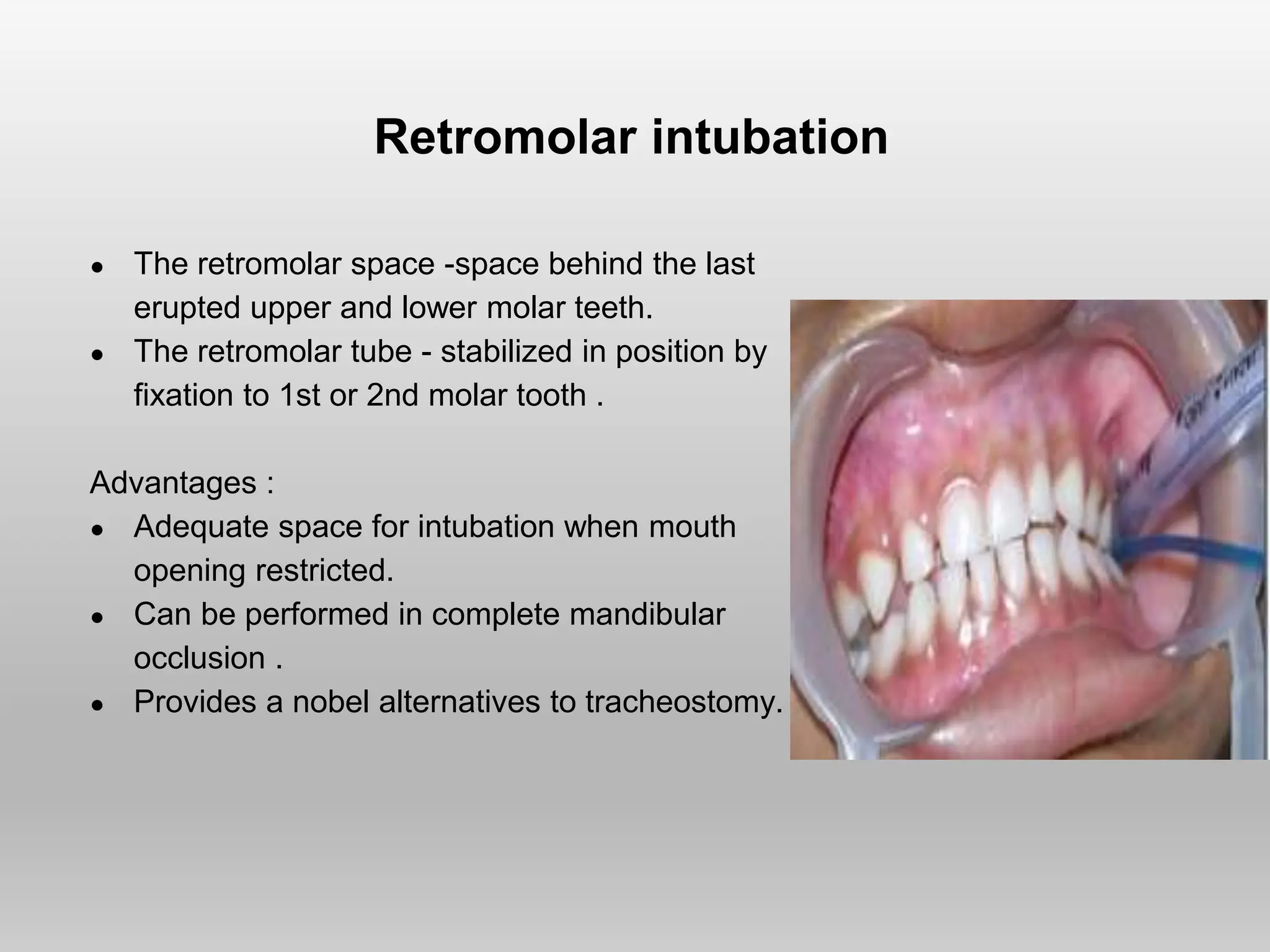
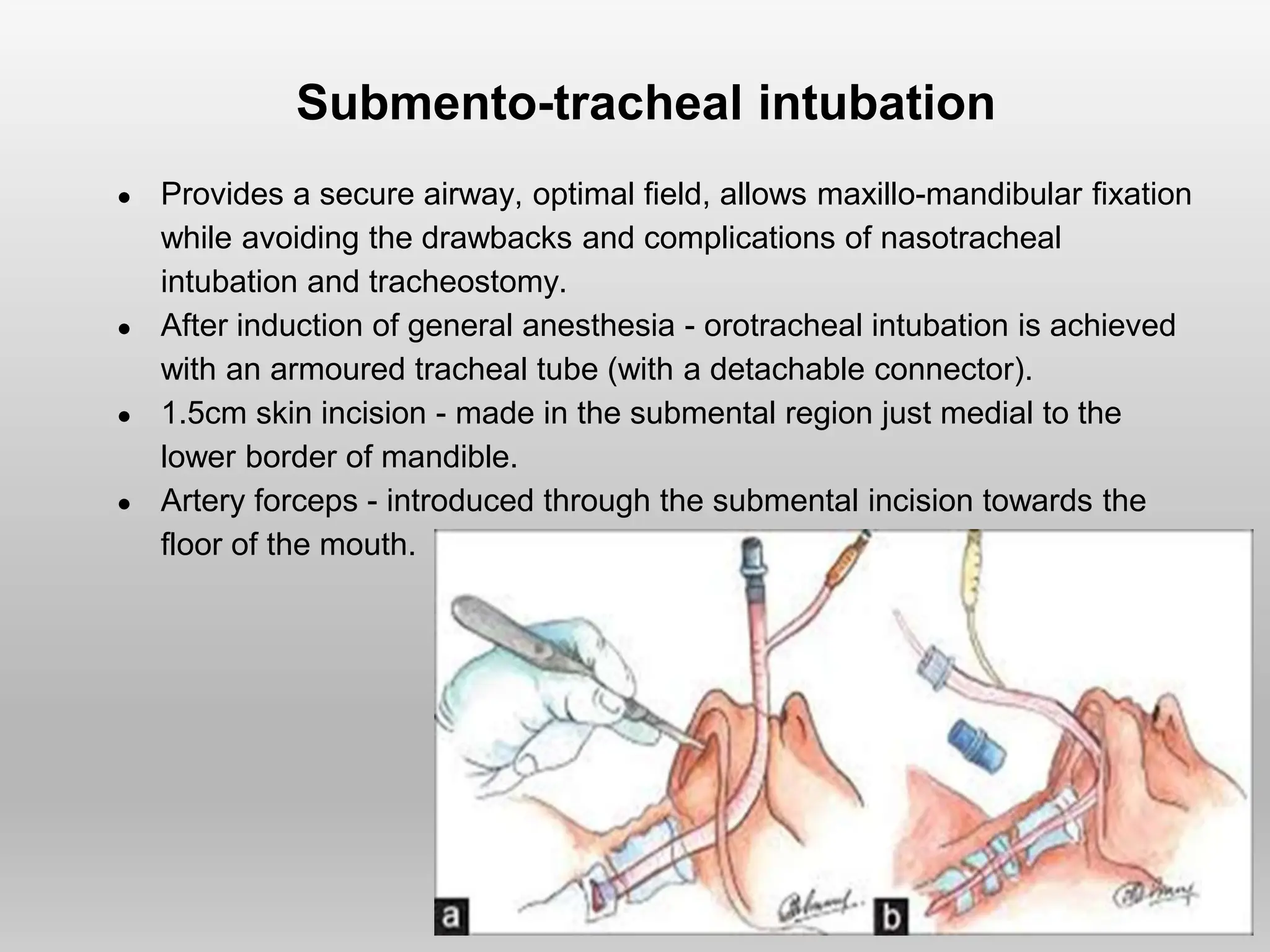
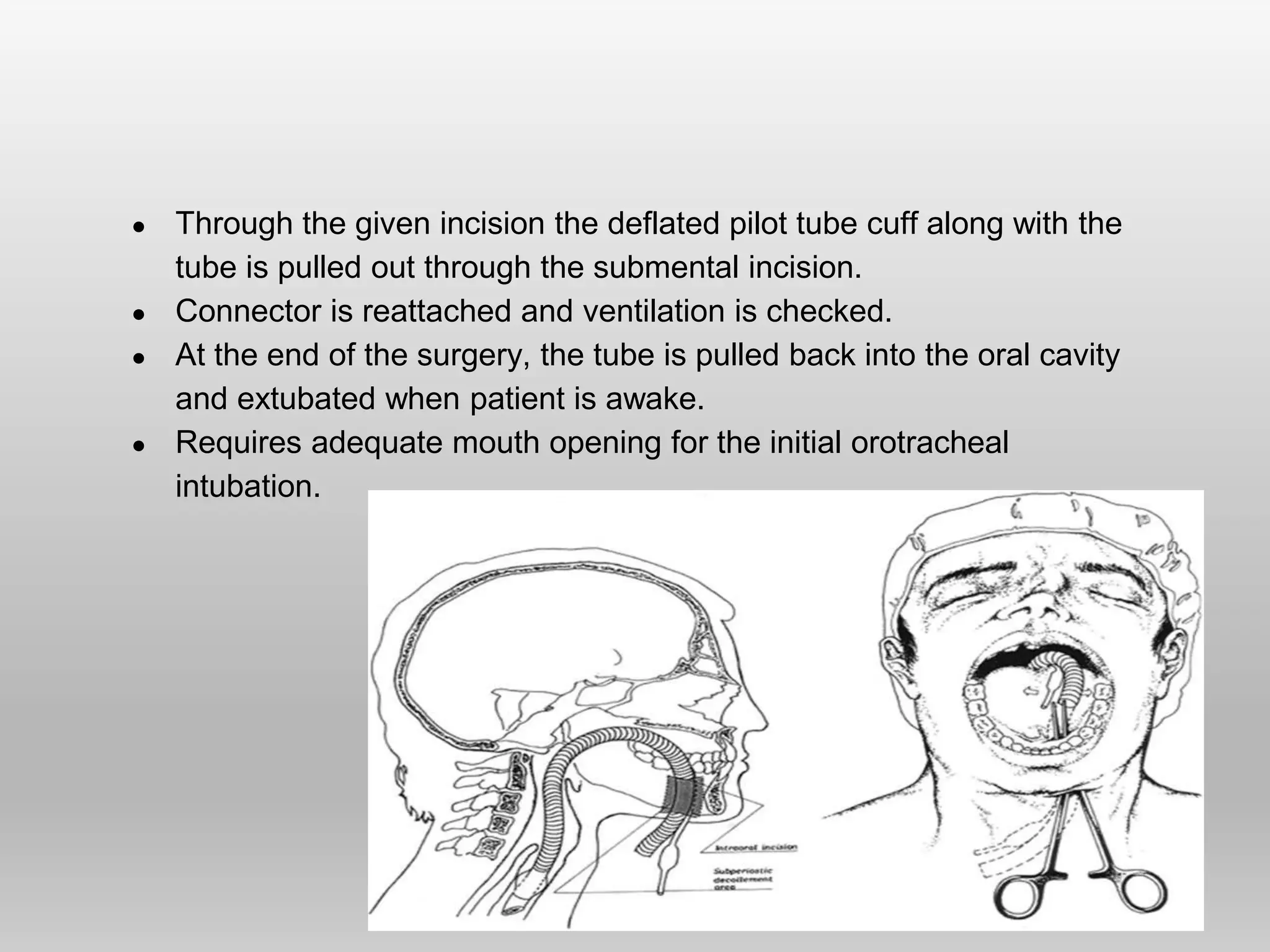
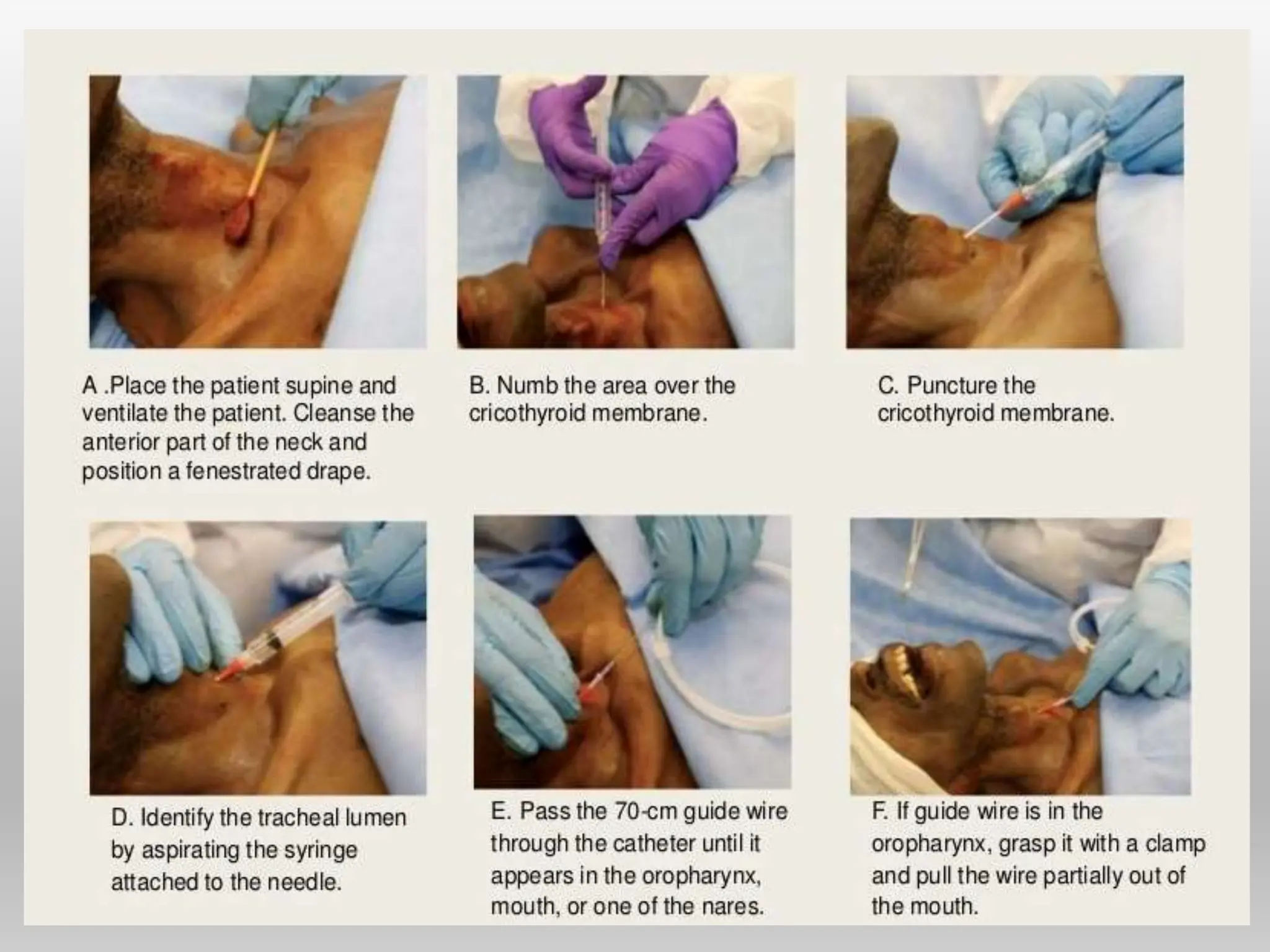
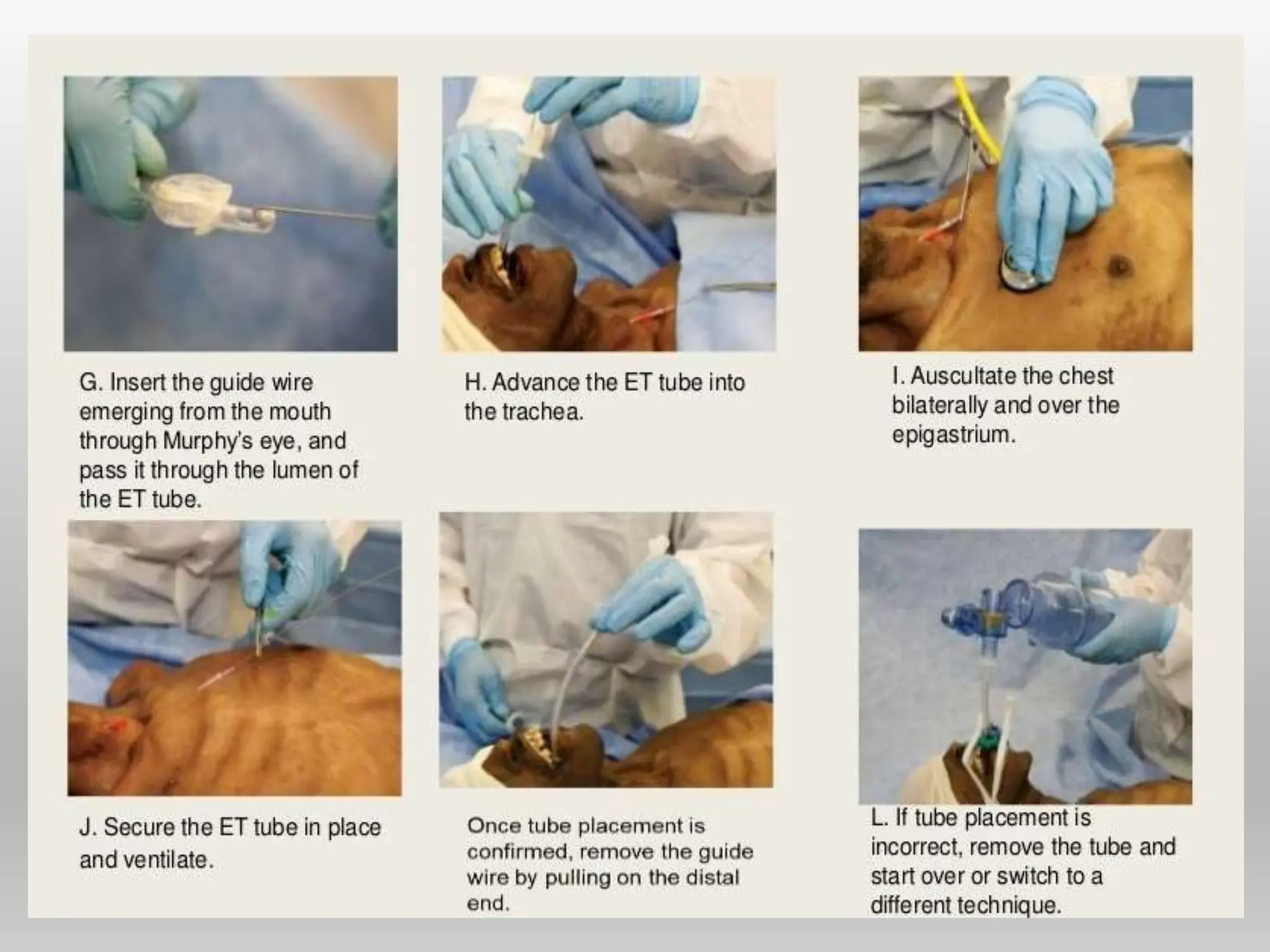
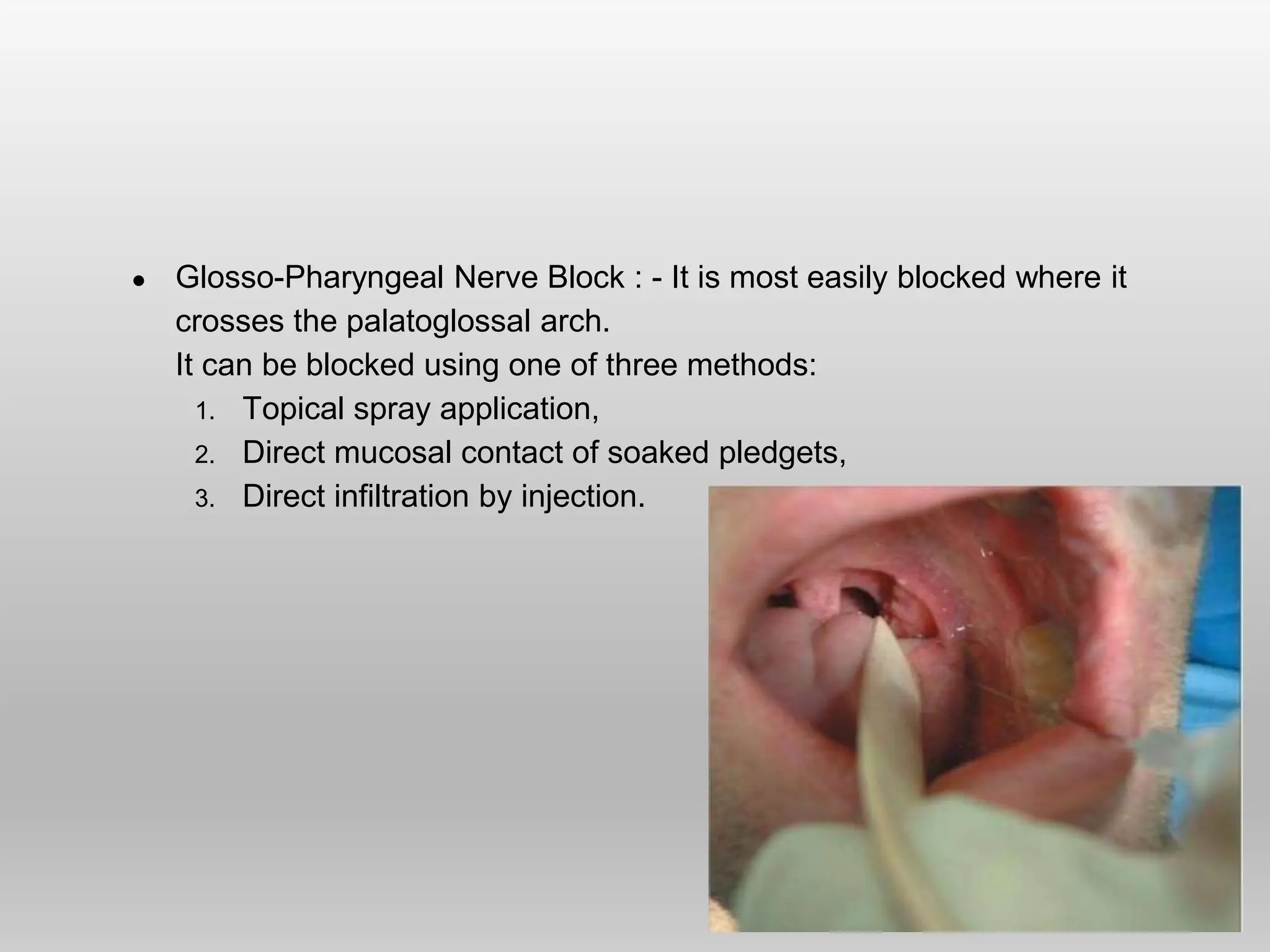
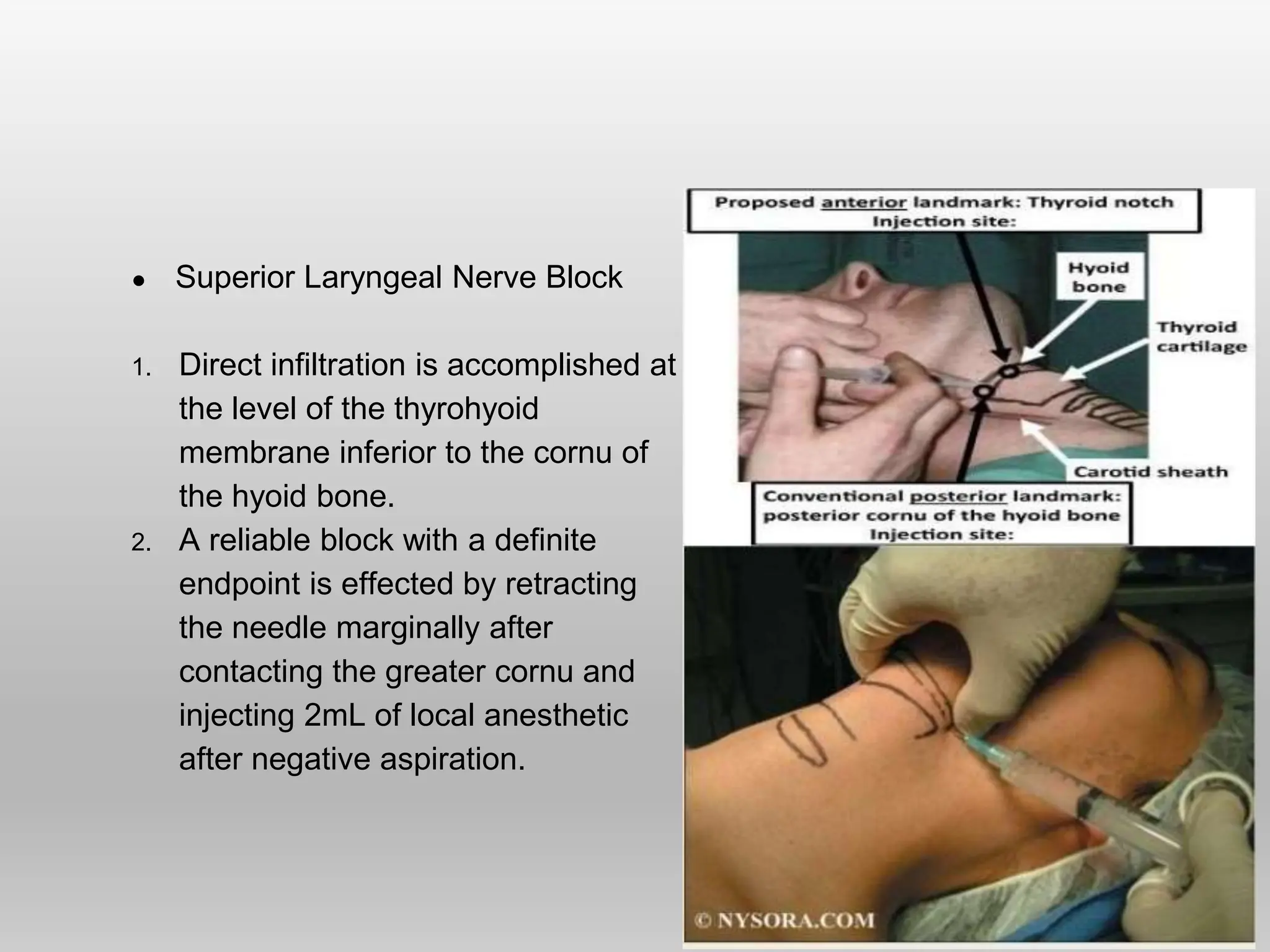
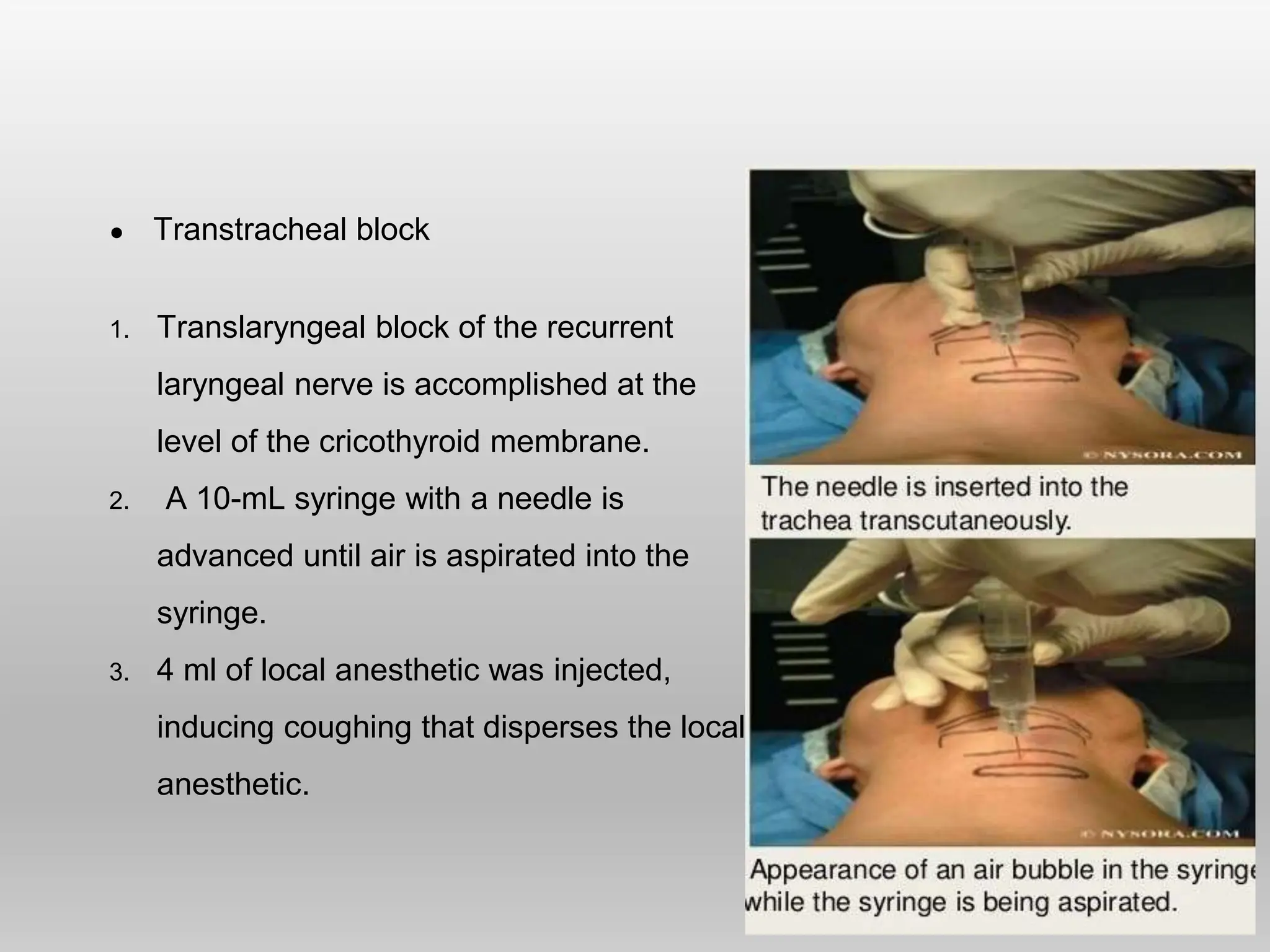
The document discusses various anesthesia techniques in dental procedures, covering historical aspects, types (out-patient, day-care, in-patient), and specific methods for local and general anesthesia. Key considerations include indications, complications, and techniques for nerve blocks, conscious sedation, and general anesthesia, as well as airway management strategies in maxillofacial surgery. Comprehensive preoperative assessments and monitoring standards are emphasized to ensure patient safety during procedures.