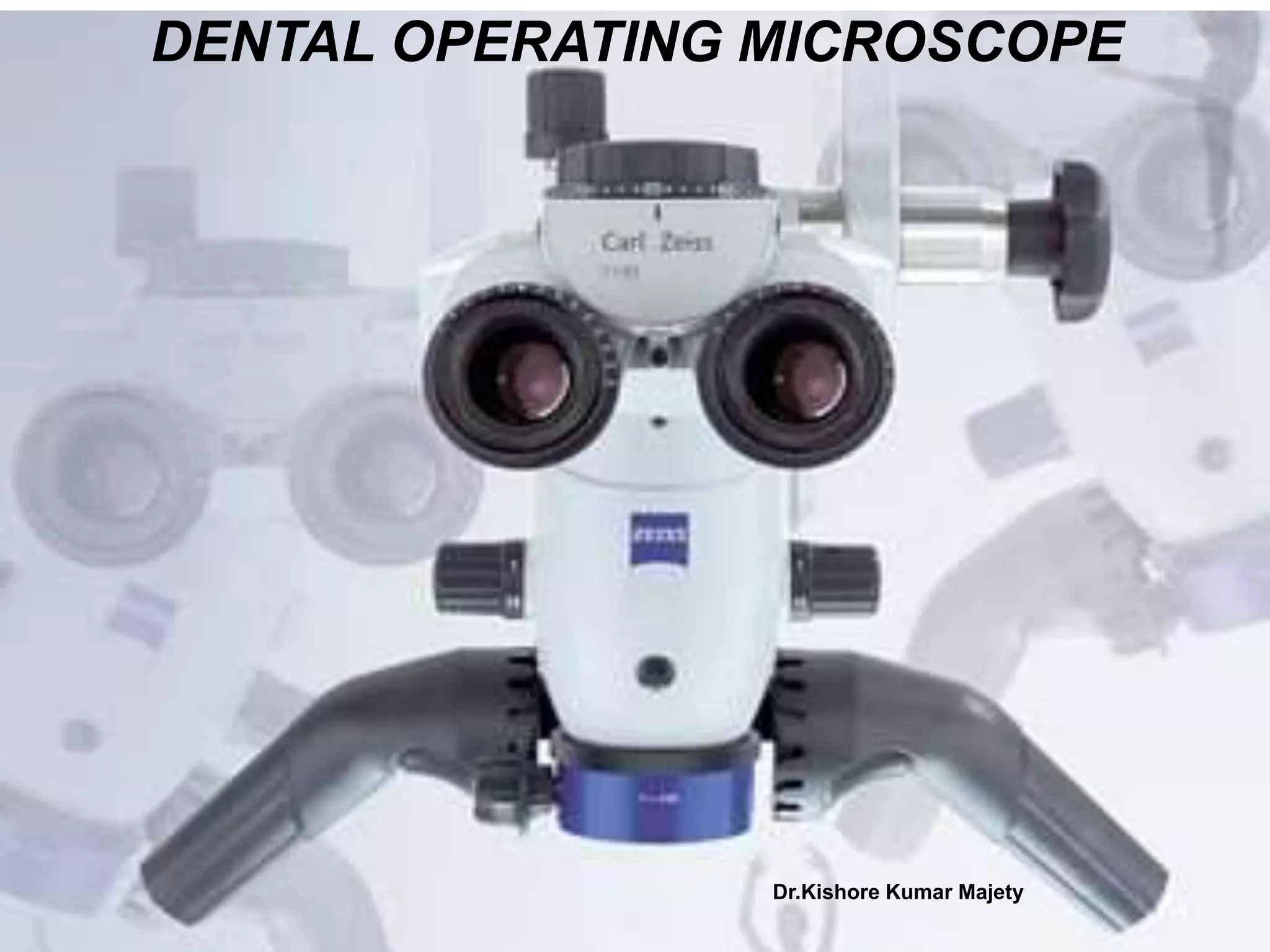
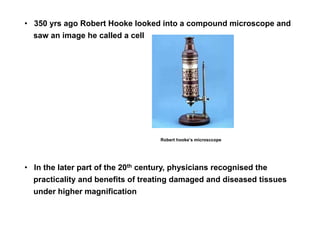
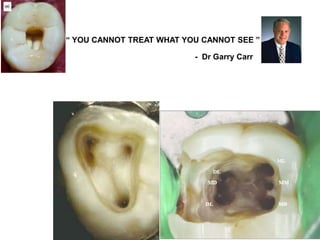
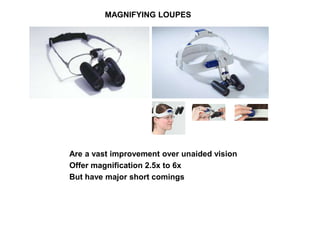
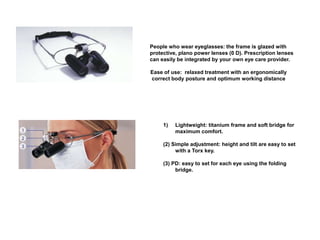
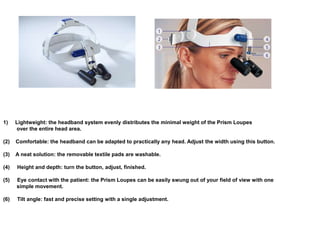
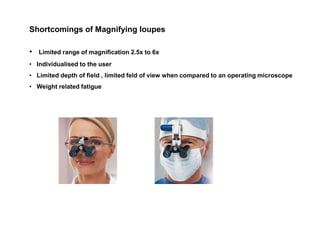
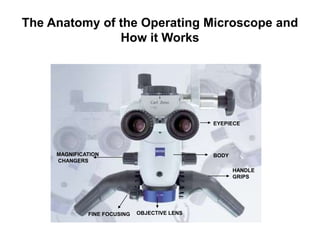
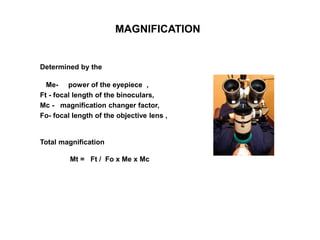
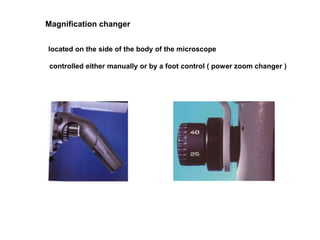
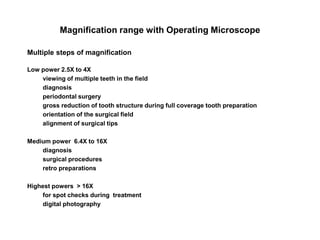
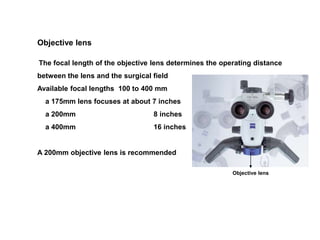
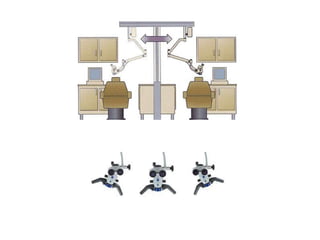
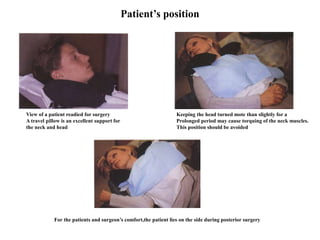
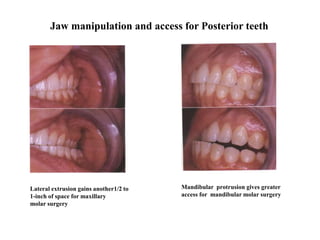
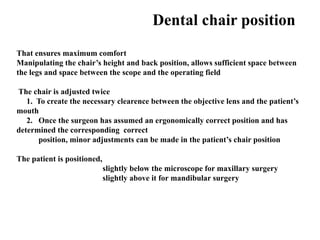
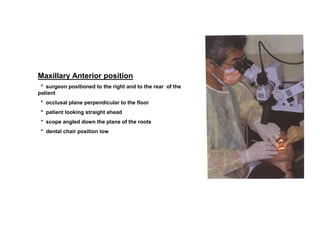
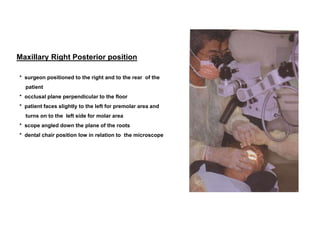
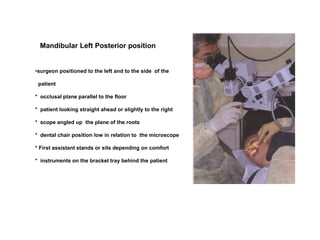
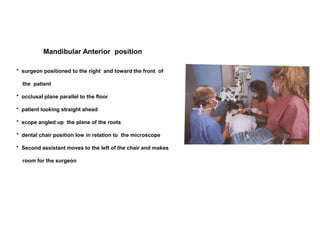
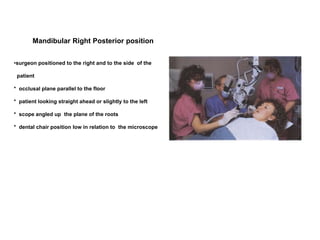
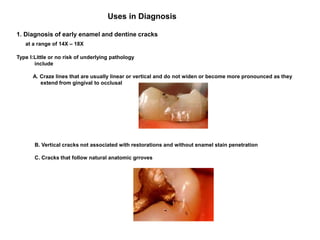
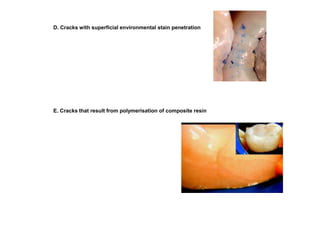
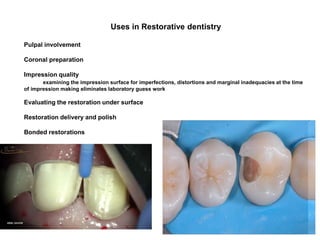
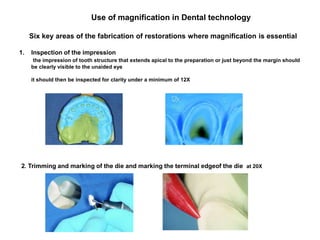
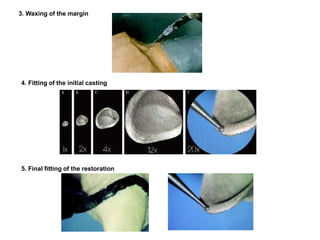
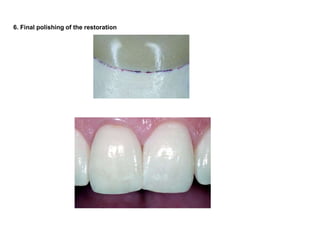
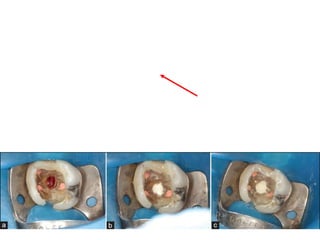
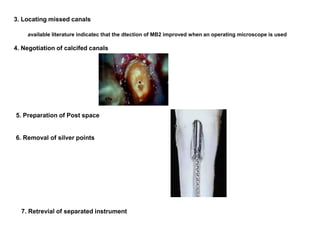
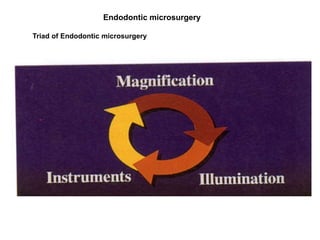
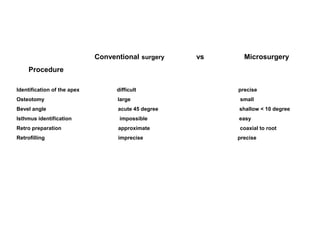
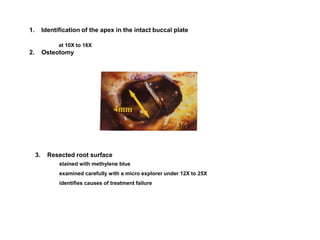
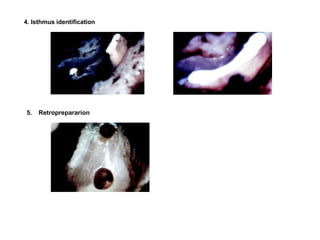
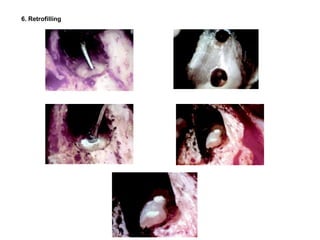
The document discusses the history and advantages of using a dental operating microscope. It describes the anatomy of an operating microscope including its magnification, illumination, and accessory components. Various configurations and operating positions are outlined. The uses of an operating microscope are explored for diagnosis, restorative dentistry, endodontics including conventional, surgical, and microsurgery applications. Benefits are seen in dental technology, patient education, documentation and enhancing dental practice.