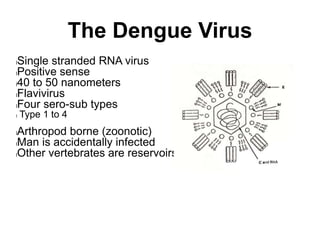
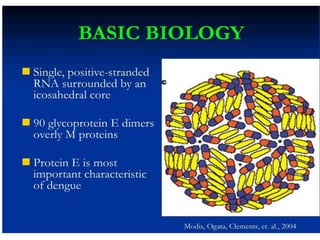
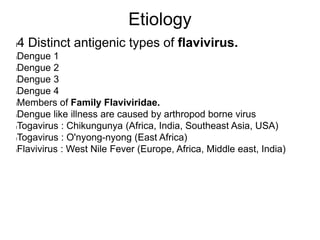
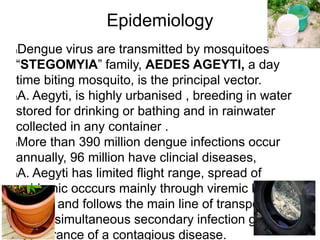
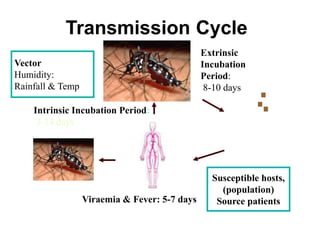
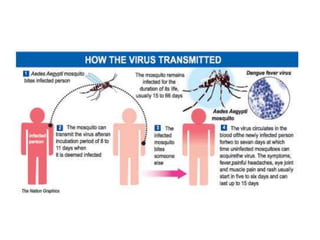
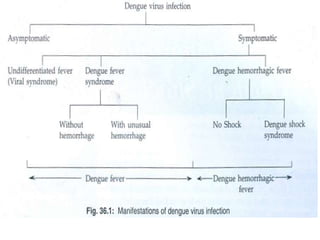
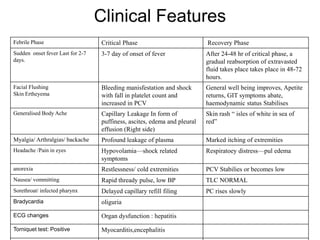
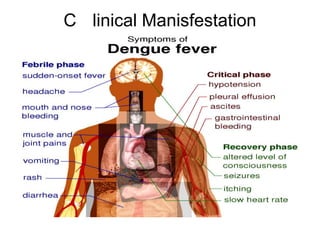
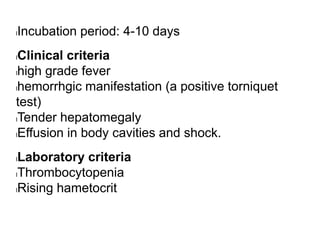
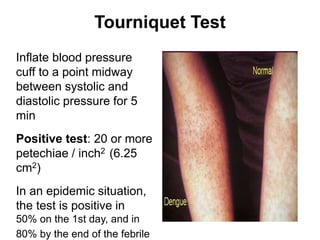
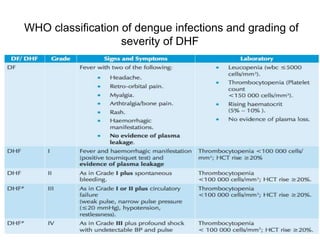
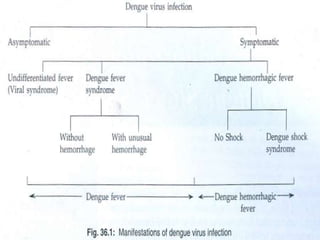
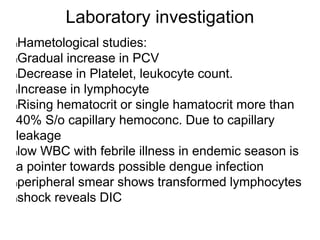
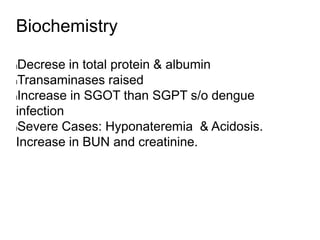
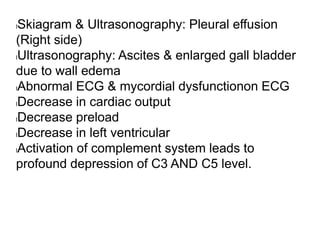
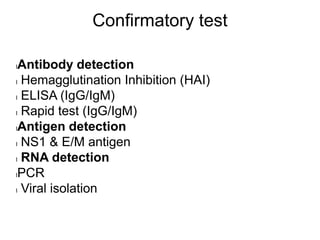
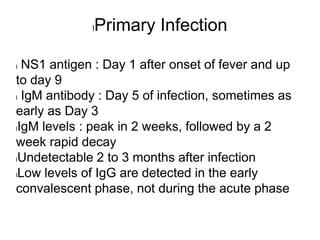
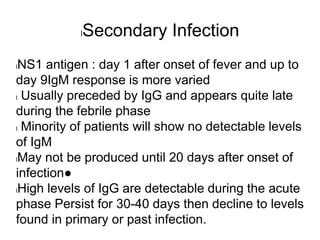
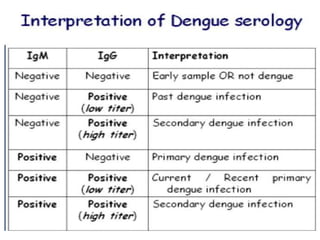
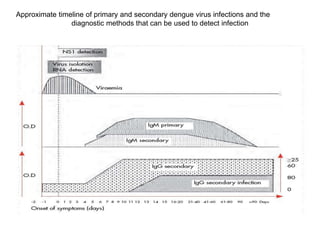
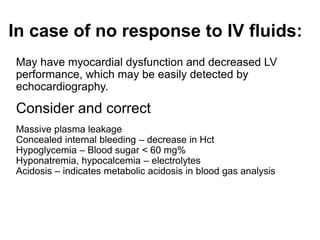
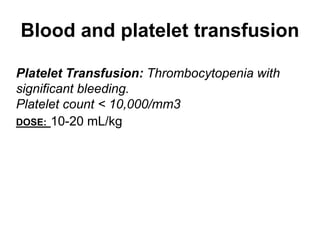
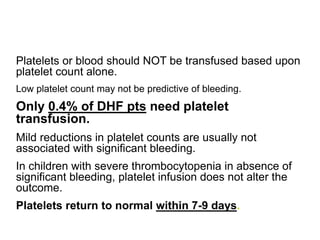
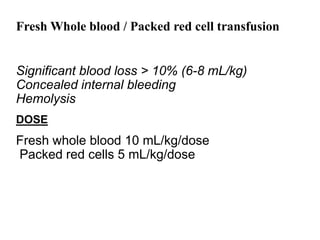
This document discusses dengue, a mosquito-borne viral disease. It causes a flu-like illness called dengue fever or a potentially lethal complication called dengue hemorrhagic fever/dengue shock syndrome. The causative agent is one of four dengue virus serotypes transmitted by Aedes mosquitoes. Symptoms include fever, rash and bleeding. Diagnosis involves detecting virus, viral antigens or antibodies. Treatment focuses on fluid replacement and supportive care. Prevention relies on mosquito control measures. Secondary infection with a different serotype increases the risk of severe disease due to antibody-dependent enhancement.