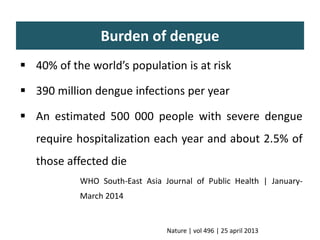
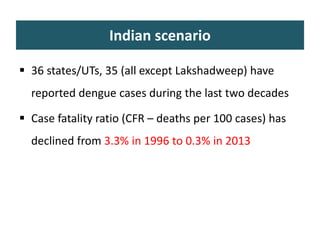
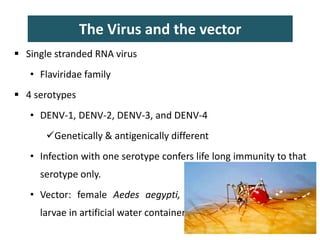
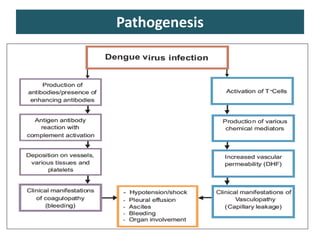
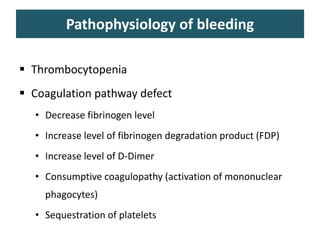
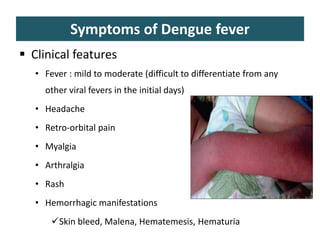
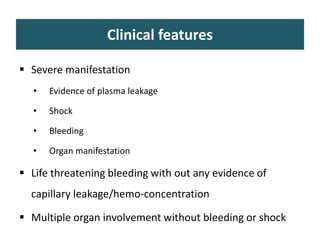
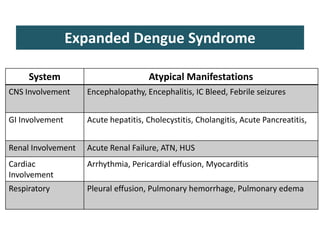
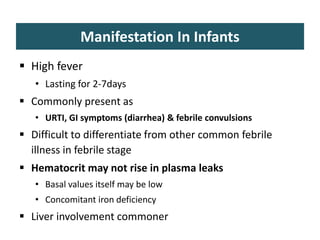
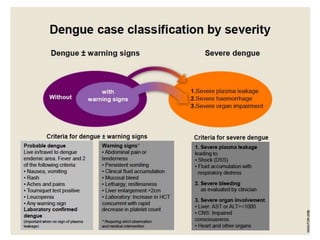
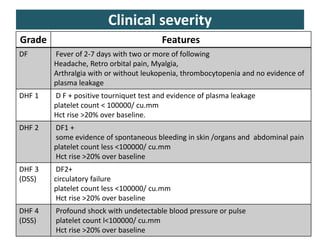
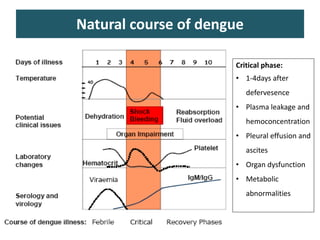
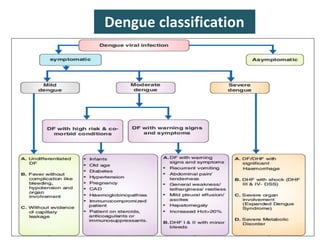
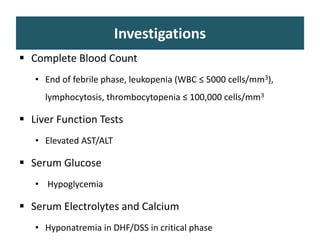
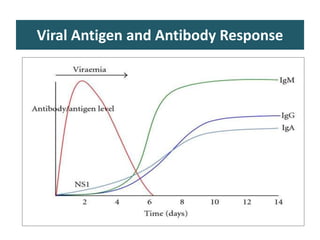
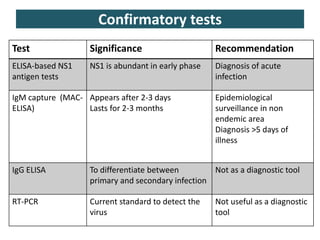
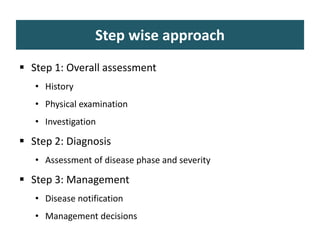
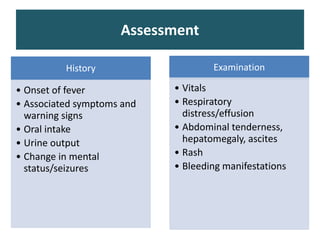
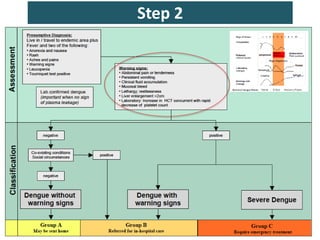
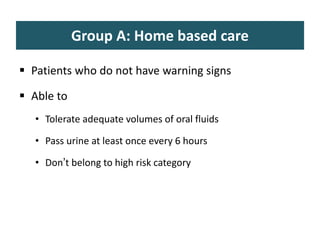
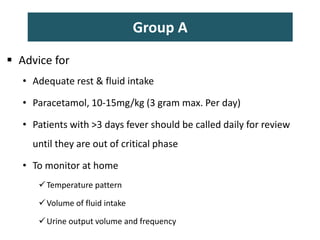
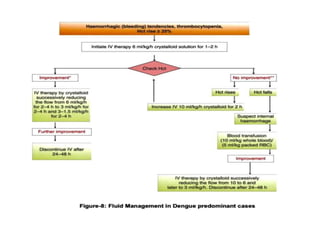
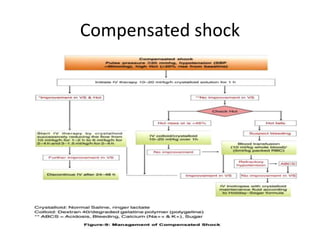
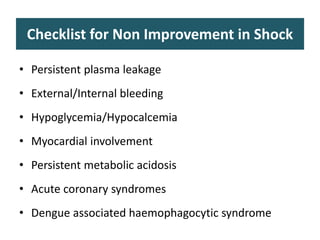
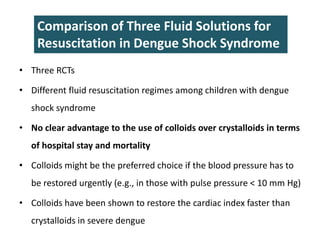
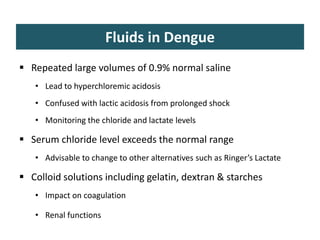
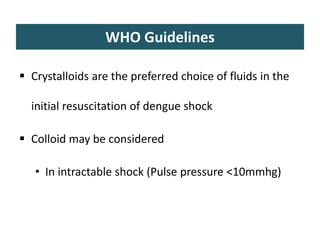
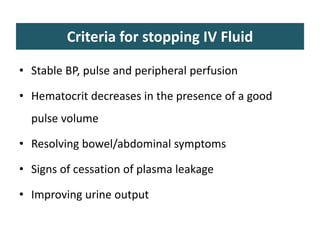
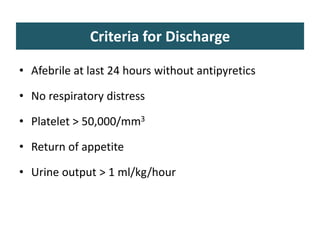
This document provides an overview of dengue fever management. It discusses the virus and vector, pathogenesis, clinical manifestations, investigations, severity grading, treatment approaches including fluid management, and discharge criteria. Key points include: dengue is caused by a flavivirus with 4 serotypes transmitted by Aedes aegypti mosquitoes; symptoms range from mild fever to potentially fatal shock; grading disease severity is important to determine management; intravenous fluids and monitoring for warning signs are the main treatment approaches.