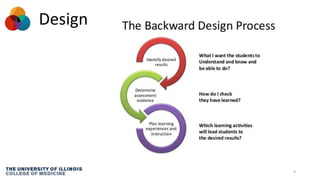
This document outlines best practices for delivering instruction in different formats such as noon conferences, mini-teaching sessions, and micro-teaching. It discusses how PowerPoint design can impact information retention and recommends designing slides with consistency, not reading slides verbatim, and citing sources. The document also suggests that observing other instructors deliver content could be an alternative to traditional evaluations. It provides tips for effective questioning during instruction and emphasizes creating a safe environment for students to answer questions.