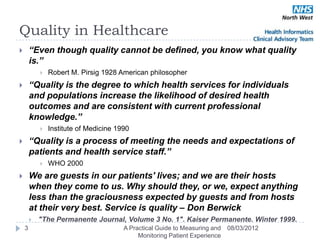
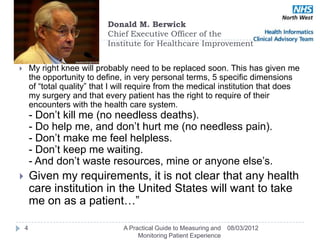
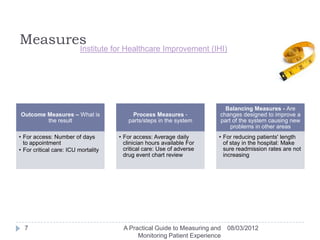
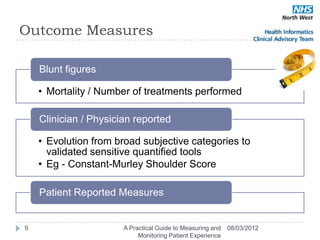
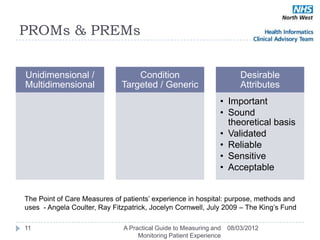
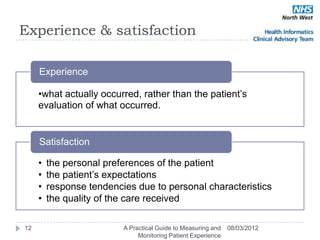
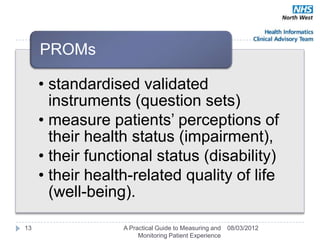
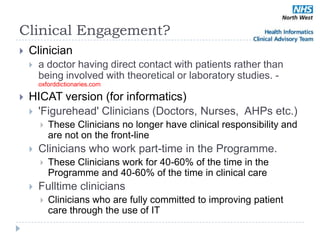
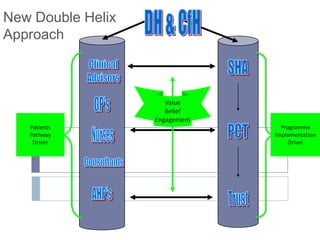
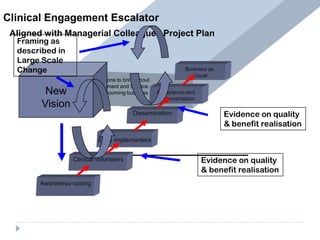
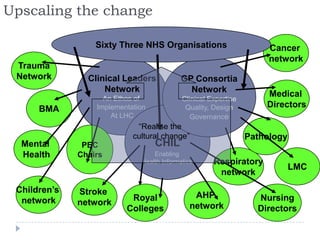
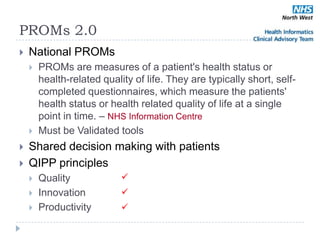
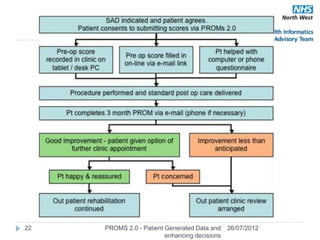
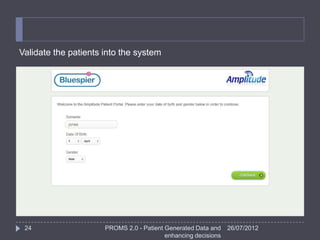
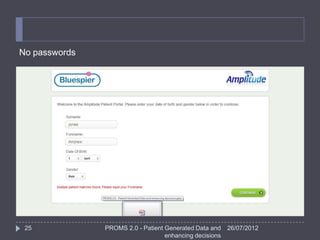
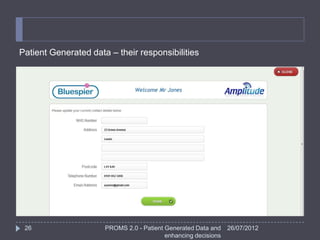
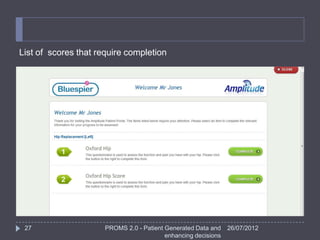
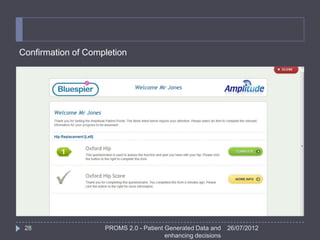
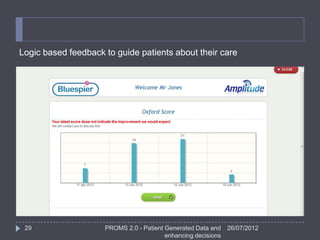
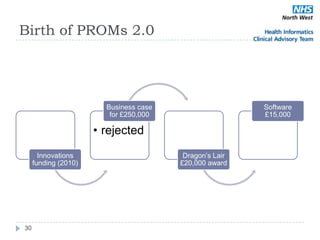
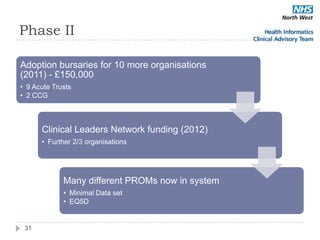
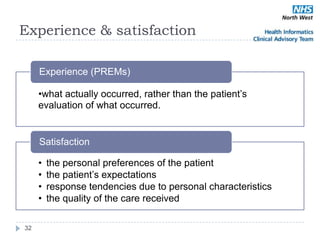
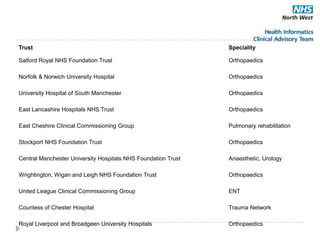
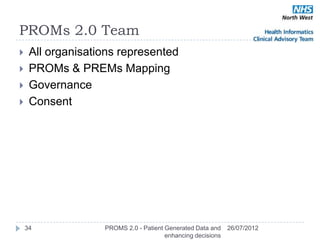
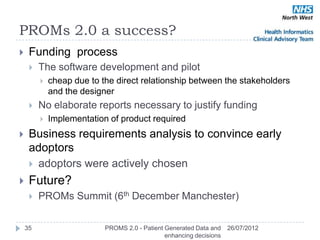
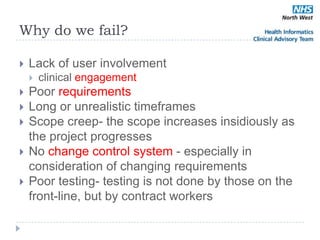
The document discusses the implementation and measurement of Patient-Reported Outcome Measures (PROMs) and Patient-Reported Experience Measures (PREMs) within the healthcare system, emphasizing the importance of quality and patient-centered care. It highlights the need for validated tools and clinical engagement to ensure successful outcomes and addresses challenges such as user involvement and project scope. The document outlines a national approach to enhance patient experience and monitoring through PROMs 2.0, which incorporates patient-generated data.